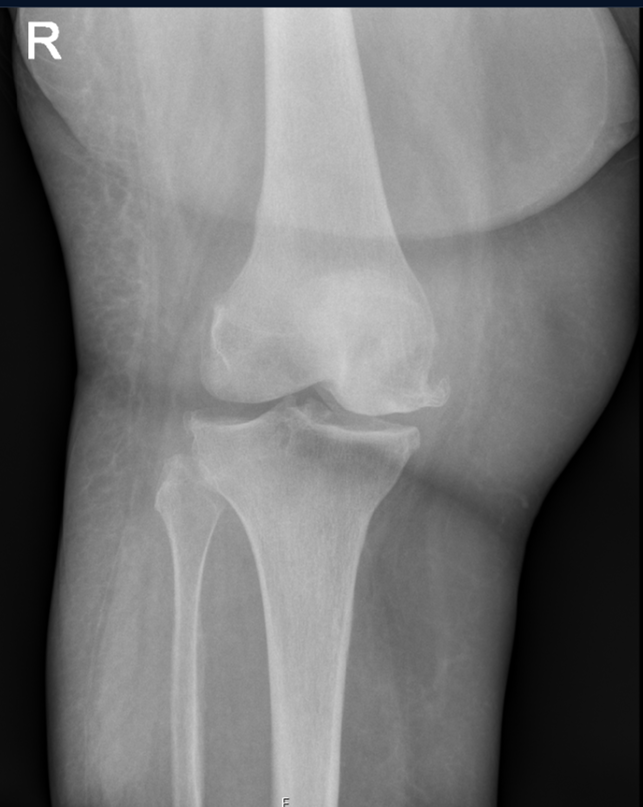
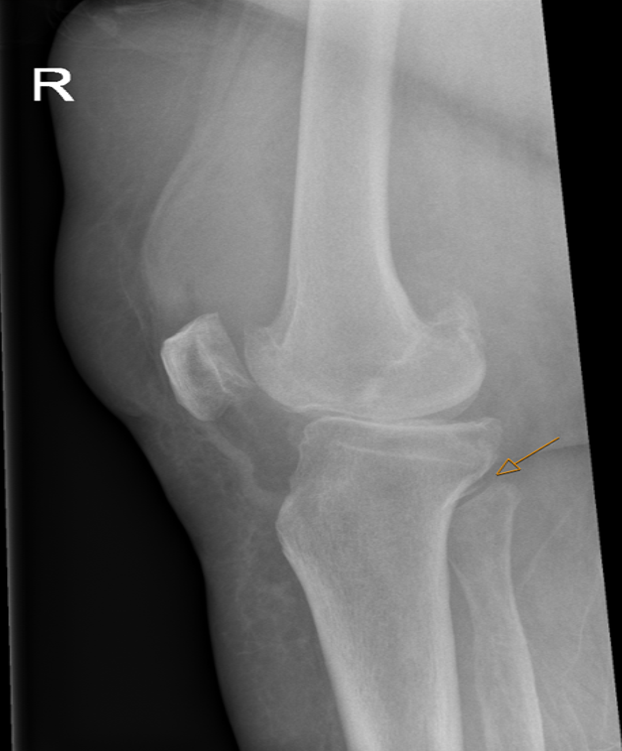
Case Presentation: Salmonella is a Gram-negative rod with multiple serotypes. This bacterium is part of resident flora of poultry, which the most common source of Salmonella. Consumption of under cooked chicken is a risk factor for Salmonella infection, which can cause invasive gastroenteritis. In less than 5% of Salmonella infections, bacteremia occurs, and more seldom endocarditis, meningitis, urinary tract infection and/or septic arthritis [1, 2]. We present in this report a rare case of Salmonella septic arthritis (SSA).A 69-year-old female with medical history of SLE and recent COVID-19 infection presented with worsening pain and swelling of her right knee for 1 week. She endorsed one day of fever up to 40 degrees Celsius. Denied any previous episodes of right knee pain, arthritis, even during active SLE periods. For SLE she takes Hydroxychloroquine and Prednisone. On exam, she appeared healthy, had hydrops of her right knee with erythema, remaining exam was normal including her other major joints. Labs showed elevated CRP of 184 mg/L, normal Cr, and CBC. X-ray of her right knee showed mild chondrocalcinosis. Aspiration the right knee revealed cloudy fluid without any crystals. Serology showed normal anti-dsDNA, C3 and C4 levels. Differential diagnosis included septic and reactive arthritis, crystal arthropathy, osteoarthritis, and COVID-induced SLE flare. She was started empirically on Cefuroxime and Gentamycin. Cultures of knee aspiration fluid and blood grew Salmonella group D, establishing the diagnosis SSA. Her antibiotic regimen was narrowed to Ceftriaxone.
Discussion: Pathophysiology of Salmonella arthritis involves invasion of small intestines, specifically M-cells, with resultant reactive arthritis secondary to microbial clearance dysfunction, involving TNF-alpha, IL-1 beta, IL-6 and IL-17, or hematogenous dissemination with resultant septic arthritis [3]. Historically, Salmonella infection rarely causes arthritis [2]. Dubost et al studied the distribution of organisms responsible for septic arthritis over a period of 20 years and found Salmonella to be a sporadic cause [1]. Groups at risk include children, immune comprised, Sickle cell disease, and SLE patients [4]. Sickle cell and SLE patients are more prone to complicated Salmonella infections, including SSA; these patients have impaired liver and spleen function, resulting in dysfunctional reticulo-endothelial system with decreased clearance of pathogens, abnormal opsonization and complement function [4]. Chen et al reported that patients with SAA, often had an underlying systemic disease including alcoholic liver disease, chronic viral hepatitis, diabetes mellitus, chronic renal disease, and most commonly SLE [5]. A large retrospective study consisting of 3127 SLE patients, found 29 cases of septic arthritis, out which 17 (59%) had Salmonella gastroenteritis [6]; 4 of 7 cases of SLE with glomerulonephritis and SSA turned out to be a chronic carrier of Salmonella in their bile, bone marrow and intestines. It is estimated that within the normal healthy population Salmonella is cleared in less than six months, and less than one percent is chronic carrier [7].
Conclusions: Invasive Salmonella gastroenteritis can cause both reactive and septic arthritis. Young patients with SLE are at a higher risk of developing SSA. Patients with active SLE, with previous confirmed Salmonella infection, should be tested for chronic carrier state for Salmonella prior to initiating immunosuppressive treatment, to reduced risk of SSA.