Background: The hospital discharge process is challenging and opportune for human error. Medication discrepancies continue to be a patient-safety problem, exacerbated with the multiple sources of discharge medication documentation. Medication discrepancies may lead to medication errors and may contribute to adverse drug events with potential subsequent healthcare utilization and cost. Discharge medications can be listed within discharge summaries (DS), patient discharge instructions (DI), or the electronically-generated discharge medication list (eDML) given to the patient in the after visit summary (AVS). Within the electronic health record (EHR) at our institution, each of these document types can contain unique discharge medication lists, creating opportunities for discrepancies. Clinicians have routinely used EHR developed links to import medication lists into DS and DI. The rates of medication documentation discrepancies at our academic institution is unknown.
Methods: This retrospective study was conducted at an academic tertiary care county hospital. We performed a randomized chart review of 239 discharge encounters with an equal number of encounters from medicine, surgery, cardiology, and ob-gyn services. Discharge encounters between January 1 and March 30, 2017 were studied. We compared medication names, number of medications, dosages, and signatures among the DS, DI, and eDML for each encounter. In April 2017, the EHR governance committee disabled many commonly used links being used to import discharge medications lists. Post-intervention, a similar retrospective randomized chart review of 240 discharge encounters was conducted. Encounters from the same services were studied between July 1 and September 30, 2017.
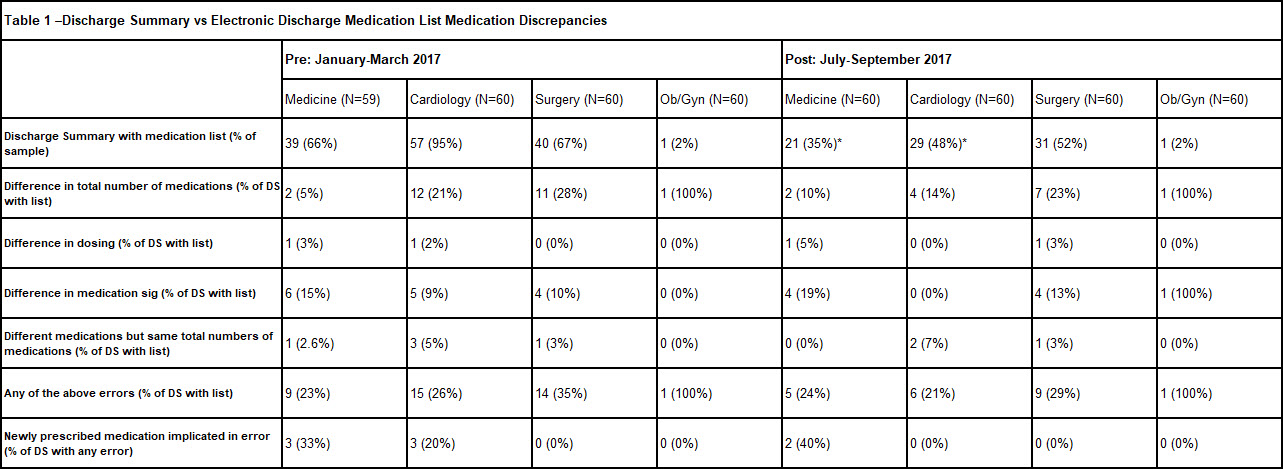
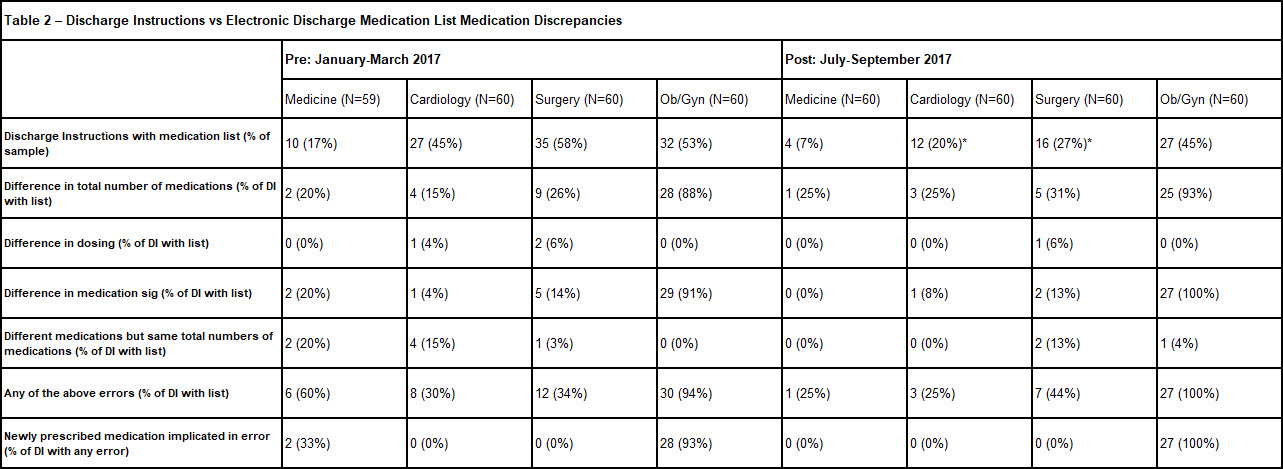
Results: Prior to the intervention, at the county hospital, 57% of DS contained a medication list, and 28% of these lists had errors. Post-intervention, these rates fell to 34% and 26%, respectively (Table 1). Prior to the intervention, 43% of DI contained a medication list, and 53% of these lists had errors at Parkland. Post-intervention, these rates fell to 25 % and 38%, respectively (Table 2). The 2 largest categories of discrepancies for both DS and DI lists were: difference in total number of medications listed and difference in medication sig.
Conclusions: No prior studies have described discrepancies between discharge medication lists generated in the EHR for the adult hospitalized population. We demonstrate that these discrepancies are prevalent within our institution, and that modifying EHR functions may reduce absolute discharge documentation errors. Patients receiving multiple lists that contain varying number of medications or different medication sigs has a high risk for leading to adverse drug events, increased costs, and increased healthcare utilization. In this study, we show the rate of discrepancies and one approach to decrease the absolute number of discrepancies by modifying EHR functionality.