Background: Nationally, inpatient medical oncology services are transitioning from services led by oncologists to hospitalist led with a consultant medical oncology team. There is national literature surrounding inpatient medical oncology services being poorly received by residents for a variety of reasons. Inpatient medical oncology is generally limited to medical complications and challenging goals of care scenarios which limits exposure to the breadth of the field, with many cases treated purely in the outpatient setting. It is also difficult to prioritize learning on these services. We set out to improve internal medicine resident learning on our inpatient medical oncology team through a standardized weekly teaching approach.
Methods: This was set at an academic medical institution with 12 internal medicine residents per year (plus preliminary interns) where two internal medicine residents (one senior, one intern) rotate per week on this required rotation. Standardized topics were selected for this initiative based on a combination of ABIM board requirements and areas of clinical significance as determined by attending hospitalists and oncologists. These topics were a combination of solid tumor types and oncologic emergencies. Thirty-minute educational sessions were prepared based on these topics using case-based learning at a dedicated weekly time. Residents were surveyed before the initiative and 6 months after initiation to assess preferences on the service and perceived knowledge on the topics. The initial 6 months phase was specifically based on oncologic emergencies, with the next phase of cases planned to include solid tumor topics. Additionally, residents were surveyed before and after their service weeks to assess the learning of that week’s dedicated topic.
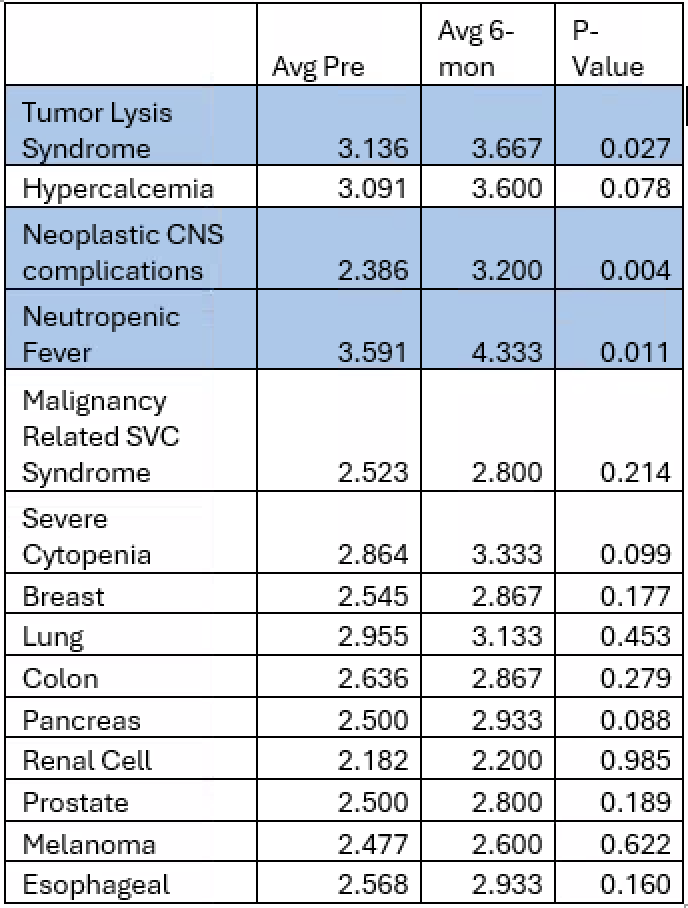
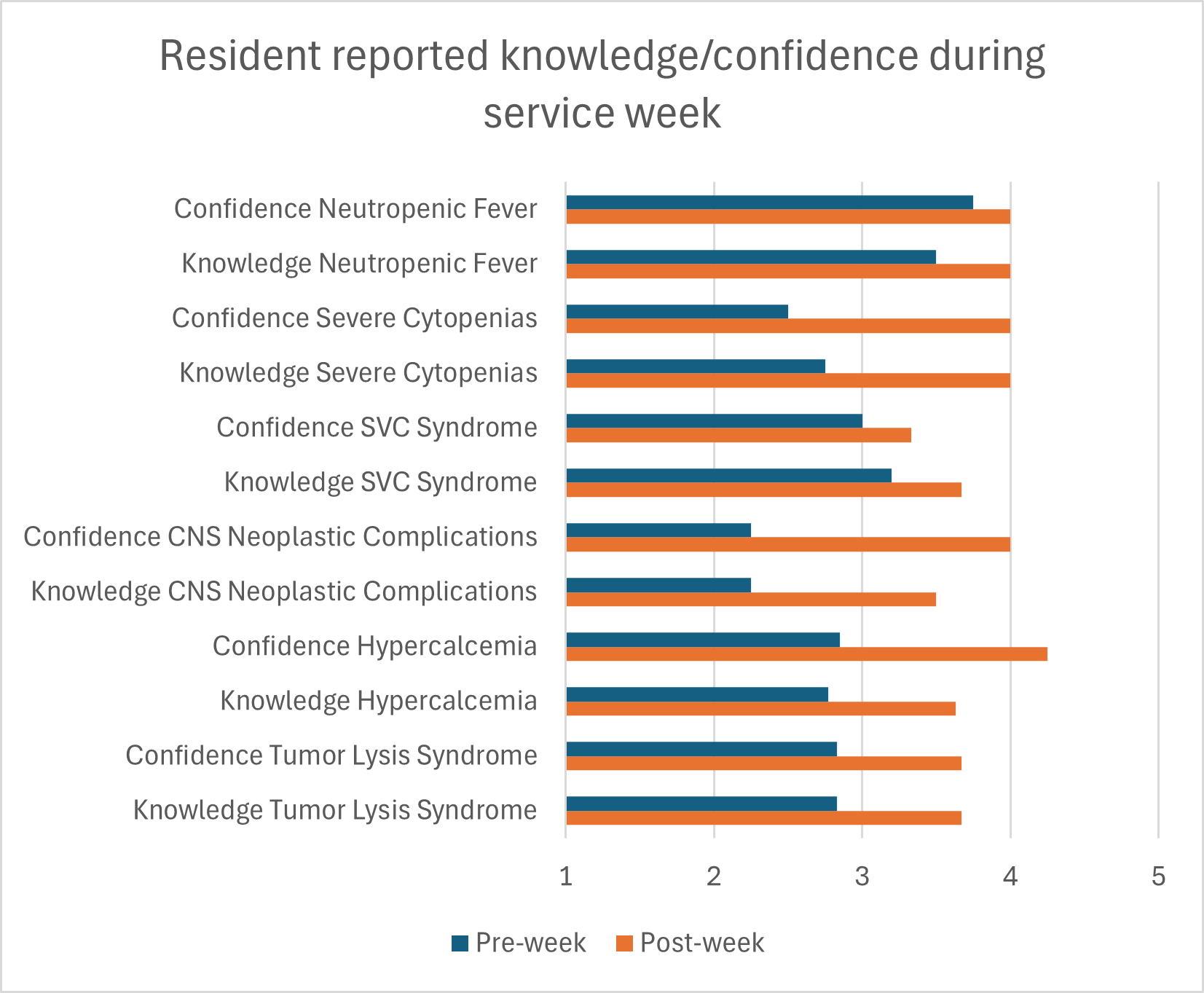
Results: 42 residents completed the pre-intervention survey, 20 completed the post 6-month intervention survey. As per table 1, there was improved self-rating of knowledge across all the oncologic emergencies, with statistical significance in 3 out of 6. There was improved self-rating of knowledge in the solid tumor topics, but none of these reached statistical significance. As per figure 1, residents consistently showed improvement from the pre to post week survey. Due to the low volume of residents rotating through in this intervention period, statistical significance of the pre to post weekly survey was not tested for. On average across the weeks, residents agreed to strongly agreed that the teaching session was valuable.
Conclusions: This teaching initiative proved to be a way to incorporate structured and dedicated learning into a busy medical oncology service, while also respecting the time needed to accomplish clinical duties. It was well received by residents, attendings and oncologists and had demonstrated improvement in knowledge obtained on oncologic emergencies while on the rotation. A similar structure is being undertaken to incorporate solid tumor topics.