Background: Decisional capacity requires four dimensions: 1) understanding of information given to make a choice 2) appreciation of situation as it relates to oneself and own situation 3) ability to engage in comparative and consequential reasoning while rationally manipulating information given and 4) ability to communicate a decision. Recently, there have been 2 main challenges to the 4-dimensional assessment method. One involves the application of an assessment as a form of medical intervention, not a clinical tool, which reinforces the stigma and distrust of the health care providers especially by members of the marginalized communities. The second set of challenges focuses on expansion of the 4-dimensional assessment beyond its scope. To help overcome some of these challenges, two aspects of decisional making capacity are required: diagnostic cause of incapacity and reassessment. While there are some studies on assessment of capacity, it is difficult to find studies on what happens once patients have been declared to have decisional incapacity. The purpose of this retrospective study was to examine how many patients have had their decisional capacity assessed (DCA) during a psychiatry consult and were then reassessed during the same hospitalization.
Methods: A retrospective review of the electronic health records of patients admitted to an urban tertiary academic institution between 03/01/2018 and 03/01/2021, aged 18 years or older and had a psychiatry consult specifically asking to assess for decisional capacity. Initial DCA was designated by the first formal capacity evaluation note per psychiatry, with re-evaluation defined by any documentation of a patient’s capacity by any physician of any specialty, including psychiatry, at least 12 hours after the initial assessment. Descriptive statistics were calculated for the decision of the initial assessment (capacity vs no capacity), whether the patient was reassessed, and the outcome of the reassessment.
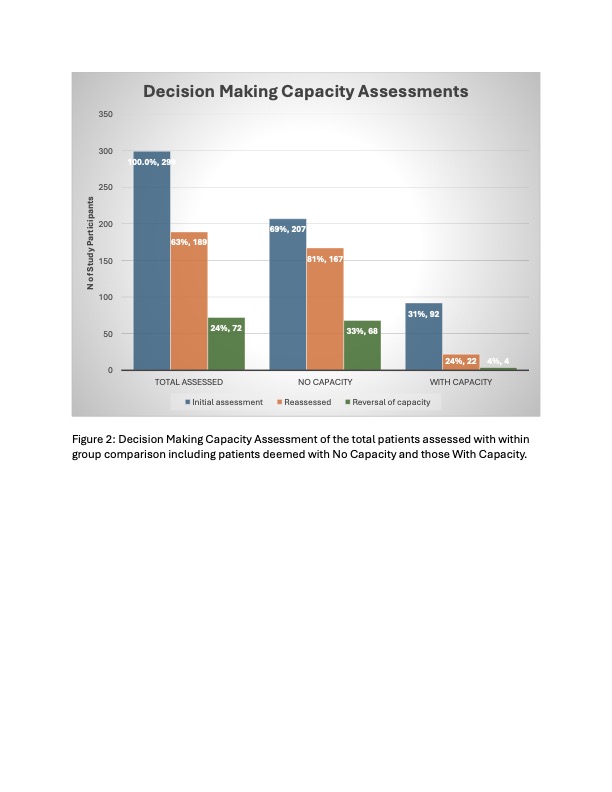
Results: There were 334 patients screened. 299 (89.5%) had their assessments completed of which 57% were male, 53% were Caucasian and 46% African American. Of the 299 patients, 189 (63.2%) had a reassessment during their hospitalization and of those, 92 (48.7%) were deemed to have no capacity, and 83 (43.9%) was deemed to have capacity. Based only on patients reassessed, of the 167 with no capacity initially, 68 (41%) had capacity at the reassessment, while of the 92 with capacity at the initial assessment, 15 (68%) retained capacity at reassessment (95% Cis (33-48%) vs (47-89%) respectively, p = 0.02). There were 124 patients no reassessed, 14 of them refused assessment or changed their mind. Of the remaining 110 (37%), 66(60%) were discharged within 48 hours.
Conclusions: Our study found that of the patients who had decisional capacity assessments done, about 40% did not undergo reassessment. And of those with no reassessment about 60% were discharged within 48 hours. While the intent of DCA is to provide a temporary and decision-specific snapshot of a patient’s ability to make informed decisions, providers may not always practice in this way. Diagnosis and reassessments can help overcome some of these challenges and of the 4 dimensions of capacity assessment by continually engaging patients during their treatment.