Background: Delays in the discharge of the hospital ward patients cause a backlog for new admissions from the Emergency Department, and transfers from the Intensive Care Units and telemetry units. This bottleneck unnecessarily increases overall resource utilization and also negatively impacts patient care and satisfaction. Therefore, our Internal Medicine Residency Program aimed through this quality improvement project, to decrease the time between discharge orders and patients leaving the telemetry and Outer-bridge ( non-telemetry) units .
Purpose: To identify barriers; to plan and implement an appropriate multidisciplinary initiative; to measure the impact of the intervention on efficiency of discharge process.
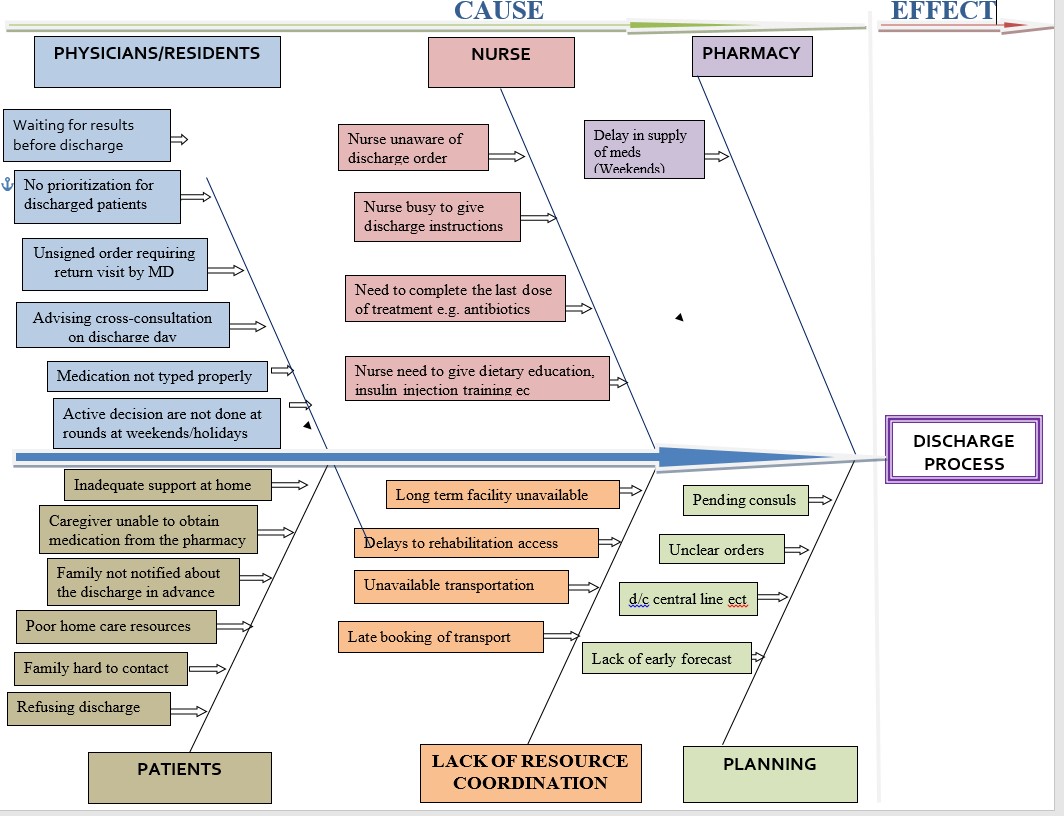
Description: A series of Six Sigma driven interventions over a period of 6 months were undertaken to uncover the root cause of the problem using the Define, Measure, Analyze, Improve and Control method. Patients included were those on the medical teaching (MTS) and on the non-medical teaching service (N-MTS), who were discharged from the telemetry and Outer-bridge units. Electronic records were used to identify the patients discharged between July 2019 – December 2019. A total of 1248 discharges were audited; 282 patients were under MTS and 966 patients were under N-MTS. The following intervention was planned and implemented. Project interventions: • Education sessions including residents, nurses, case managers, and the units’ secretaries. • Adding a new tab” Discharge Planning” under the tasks in the resident hand off emphasizing planning the discharge in advance. • Daily Tiger Text (protected clinical communicating tool) reminder to the teams to identify in advance the patient for possible discharge • Attending daily multidisciplinary rounds and biweekly meeting with expediting the discharge process committee. • Analyzing daily report obtained with the help of IT • Sharing data with the teams for feedback to improve performance, focusing on positive reinforcement. Endpoints of the study: • Discharge process Time (DpT) for all the patients pre and post-interventions • DpT of the MTS patients before and after intervention. • Identifying the time-frame window, with the most efficient DpT.
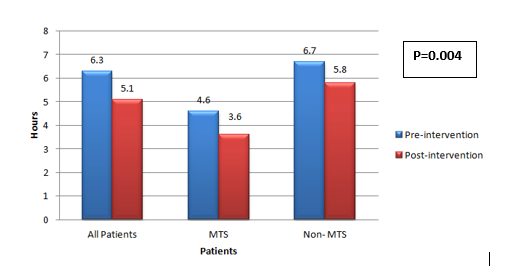
Conclusions: There was an overall statistically significant improvement in DpT post-intervention (from 378 minutes to 306 minutes, p= 0.004). DpT for the patient under MTS decreased by 22%, from 276 minutes pre-intervention to 216 minutes post-intervention, (p <0.05). DpT of N-MTS patients demonstrated a non-statistically significant trend towards improvement. Discharge before noon is an important indicator for hospital throughput. In subset analysis, DpT for MTS patients discharged before 11 am improved from 390 minutes to 234 minutes (p=0.00). DpT for N-MTS patients discharged before 11 am was not significant. The most efficient timeframe to discharge the patients was the midday (11:00-15:00) and late day (5:00-19:00). Patients discharged in morning (7:00-11:00) had a significant longer DpT (p=0.001, CI 95%).We have described an effective, resident driven multidisciplinary initiative in a community-based teaching hospital that led to improved efficiency through the hospital. While the study only evaluates improvement in discharge process as an end point for the initiative, our approach demonstrates the potential to serve as a template for assessment of more concrete outcomes such as improvement in overall patient care and satisfaction.