Case Presentation: A 25-day old, full term male, presented to the ED with one day of decreased oral intake and a rectal temperature of 39.2ºC.In the ED, the patient was febrile to 38.6 ºC and had mottled skin with an otherwise unremarkable physical examination. Initial workup included CBC with a WBC of 3.6 10^3/uL, ANC of 2240/uL, and a CRP of 13.4mg/L. A metabolic panel, urinalysis, abdominal XR and chest XR were unremarkable. The patient was started on intravenous fluids and acetaminophen for supportive management. Antimicrobial agents were not initially started and the patient was admitted to the pediatric floor. Shortly following admission, the patient had a worsening exam with persistent fevers, red mottled skin, decreased capillary refill, and increased somnolence.A lumbar puncture was performed and CSF studies were notable for a RBC of 2,840 cell/mm^3 (traumatic tap), WBC of 7 cells/ mm^3, protein of 55 mg/dL and glucose of 52mg/dL. Empiric antibiotics were started and the patient was transferred to the pediatric ICU due to concerns of compensated septic shock. The meningitis/encephalitis panel resulted positive for human parechovirus within a few hours. Following this, antimicrobials were discontinued and the patient returned to the pediatric floor after approximately 24 hours when found to be hemodynamically stable. The patient continued to improve with supportive management and was discharged on hospital day 5.
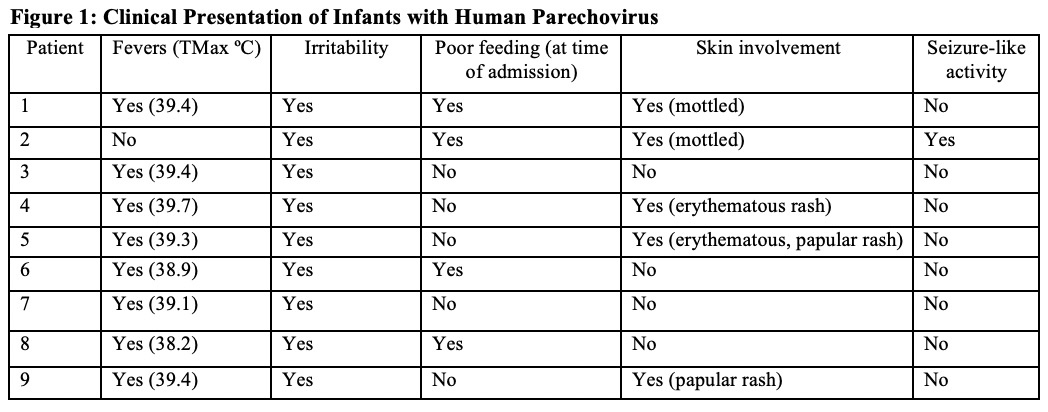
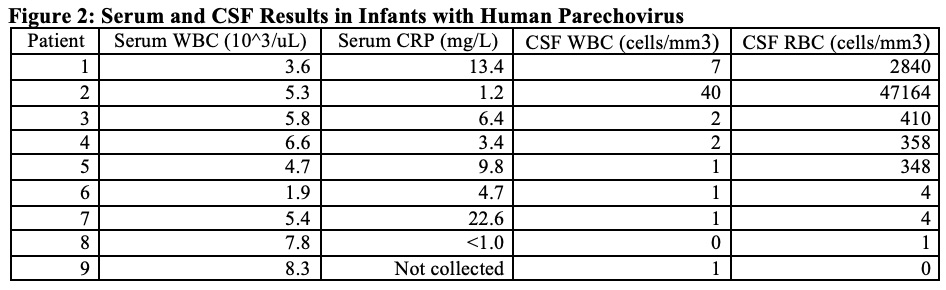
Discussion: Human Parechovirus has had increasing prevalence in the community recently with increased cases of meningitis. The viral infection has a wide range of clinical presentations with the most severe tending to be in young infants under 3 months old. The CDC issued an advisory in July, 2022 which advised clinicians to consider parechovirus in infants with a sepsis-like clinical picture, fever and signs or symptoms of meningitis or meningoencephalitis. This case is one of many with PCR-confirmed parechovirus meningitis our institution has cared for over a short period of time with varying presentations, but the majority having high persistent fevers, mottling and erythema of skin, and irritability (Figure 1).These patients often have reassuring labs and inflammatory markers despite appearing clinically ill. CSF studies also often lack pleocytosis which is atypical for most forms of meningitis but more common with this infection (Figure 2). Prior studies have shown a range of outcomes but some with development of significant developmental delay and other neurologic sequelae. Often, the only way to diagnose this infection is via PCR specifically looking for infection.
Conclusions: Parechovirus meningitis has increasing prevalence in the community. While many patients improve with supportive management, there are concerns for chronic neurologic sequelae that may develop in the long-term. Also, this infection has atypical findings compared to other forms of meningitis due to lack of CSF pleocytosis and need for specific PCR testing to diagnose. Based on this, many cases may be missed, especially in the setting of recent updates in clinical practice guidelines for febrile infants which rely heavily on inflammatory markers that are often not elevated in this illness. More studies are needed to evaluate if patients are at increased risk for long-term effects of infection and what screening and other follow-up are appropriate. Hospitalists should be aware of this as a possible infection when caring for persistently febrile infants with no other clear etiology and consider testing as appropriate.