Background: Patients feel “uncomfortable, vulnerable, and exposed” in their gowns while providers are distressed at seeing and caring for their fellow human beings clad in sub-human “threadbare,” “ugly” garments. The purpose of this study was to create a patient gown based on design suggestions by patients and providers (physicians and nurses) and to refine the novel design through clinical use and feedback from users.
Methods: Semi-structured 1:1 standardized interviews were previously conducted with 10 patients, 10 nurses, and 10 physicians at a large academic medical center to understand the attitudes surrounding the patient gown and receive input on a “patient-guided, provider approved” inpatient garment. Stemming from this work, a novel inpatient attire called “U MATTER” was developed and showcased at the Hospital Medicine 2019 “Shark Tank,” garnering feedback from hospital management and executives. Over the last 6 months, U MATTER has undergone several quality improvement (QI) cycles with input from the president of the health system, vice president of linens services, the hospital linens vendor, a professional seamstress, radiology, and health physicists.
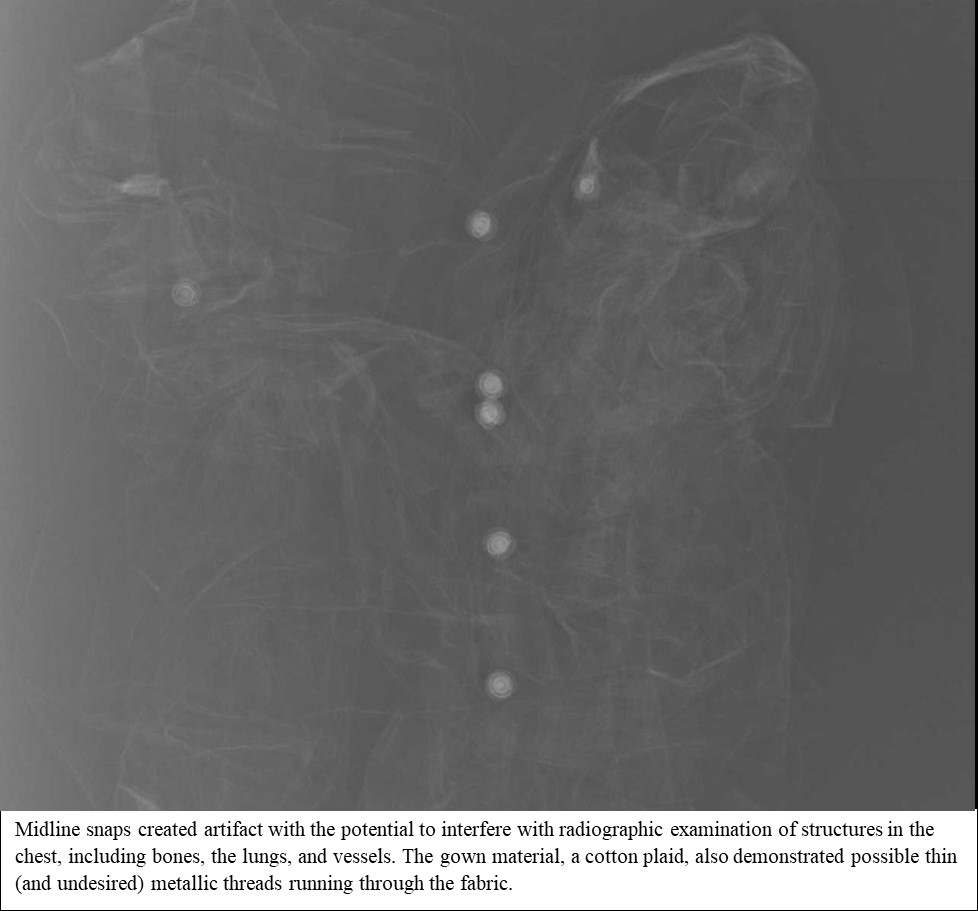
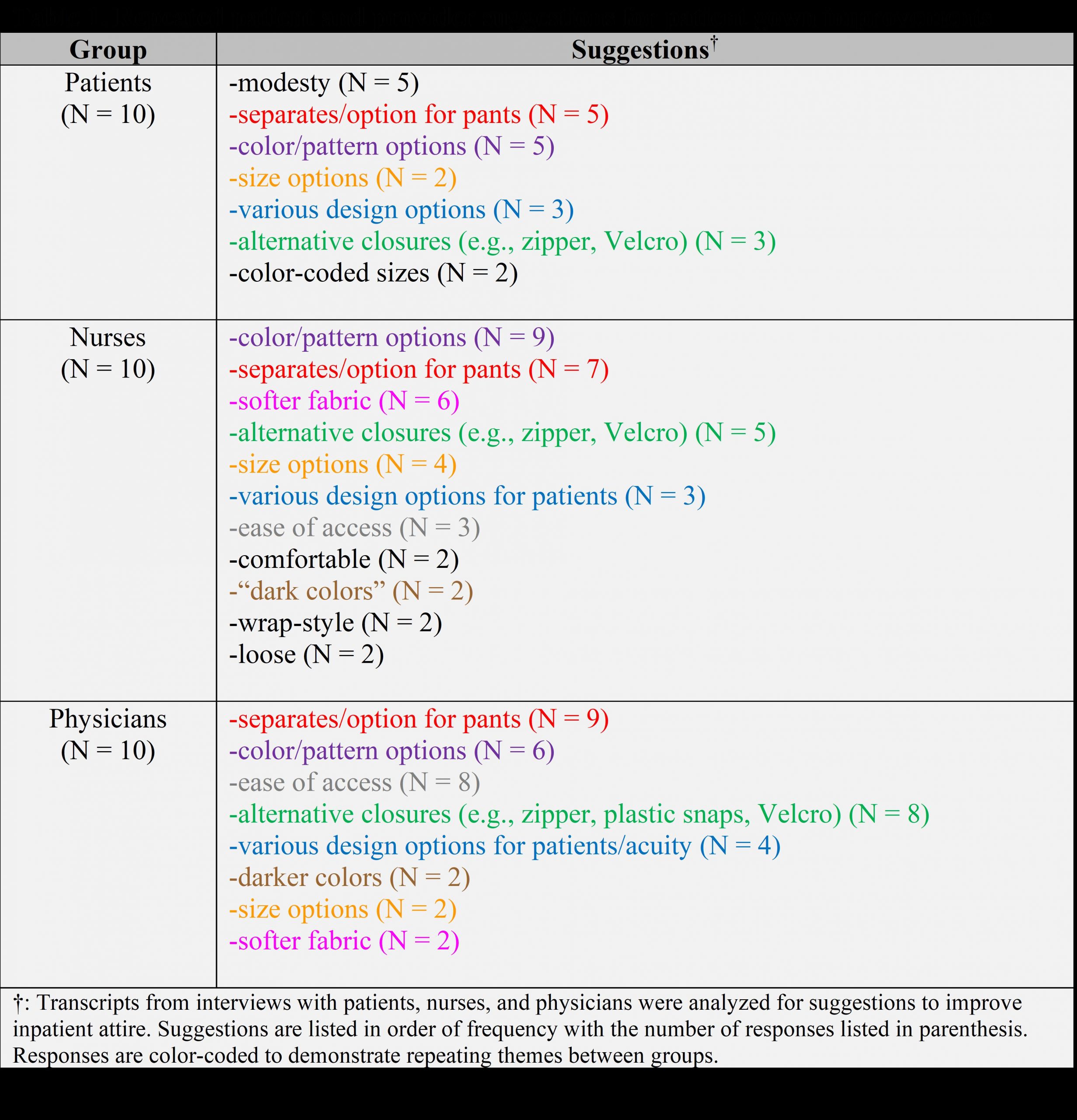
Results: Recurring participant suggestions for patient gown redesign can be found in Table 1. Among patients interviewed, the top three suggestions for patient gown improvements were: modesty, separates/option for pants, and color. The top three suggestions from nurses were color options, separates/option for pants, and softer fabric. The top three suggestions from physicians were separates/option for pants, color options, and ease of access.Keeping these results in mind, U MATTER was design to include: a faux collar with an access point for central lines/ports; a petal sleeve enabling patient independence in donning/doffing the gown; double-backed construction; a snap-line down the front of the gown to improve exam access and minimize exposure; and a soft, pineapple print jersey fabric.After undergoing QI cycles, several changes were made to the evidence-based design. First, the fabric was changed from jersey to cotton-polyester blend to be able to withstand laundering at 170F. Additionally, the snap line was removed from the front of the gown after an x-ray revealed significant artifact (Image 1). MRI confirmed compatibility of the garment. Thus, an alternative snap-free front-closure with a double-backed rear flap resulted. In looking forward to mass-production, the gown pattern was reduced from 10 pieces to 4, and the number of snaps was halved. The faux collar was eliminated as it was found to be a potential hindrance, and the opening did not sit at a level conducive to its intended purpose of port access. Finally, the pant was modified from a closed drawstring-waist to an open drawstring-waist with Velcro closure to enable ease of donning/doffing and accommodate catheterization.
Conclusions: In progressing through the QI cycles, the patient and provider suggestions drove this evidence-based refinement of the design, which will undergo pilot-testing in January 2020 at an outpatient radiology center. For one month, we will ask patients and providers to provide feedback on the latest design using a brief survey inventory that checks for ease of use, comfort, impact on morale, and pragmatics. The current U MATTER design has the option of a single colorful gown and/or quirky pajamas and is compatible with mass-production, hospital-laundering, and multimodal imaging in design and construction.