Background: Given the shift-based nature of modern hospital medicine, block schedules where physicians are on clinical service for a defined period of time are common place. As such, end-of-service handoffs are a routine element of hospital medicine practice. Like handoffs to an overnight cross-covering physician, end-of-service handoffs pose a risk to patients if critical information is not conveyed effectively (1). For hospitalists themselves, this transition also presents a challenging workflow with many physicians characterizing the “first day on service” as the most difficult day of their service period. With many hospital medicine groups focusing on length of stay reductions, ensuring seamless service end-of-service handoffs that incorporate discharge planning elements is also important (2).
Purpose: The aim of this project was to design a standardized end-of-service handoff to minimize risks associated with transitions of care, improve the ease of practice in hospital medicine, and provide continuity with regard to ongoing discharge planning.
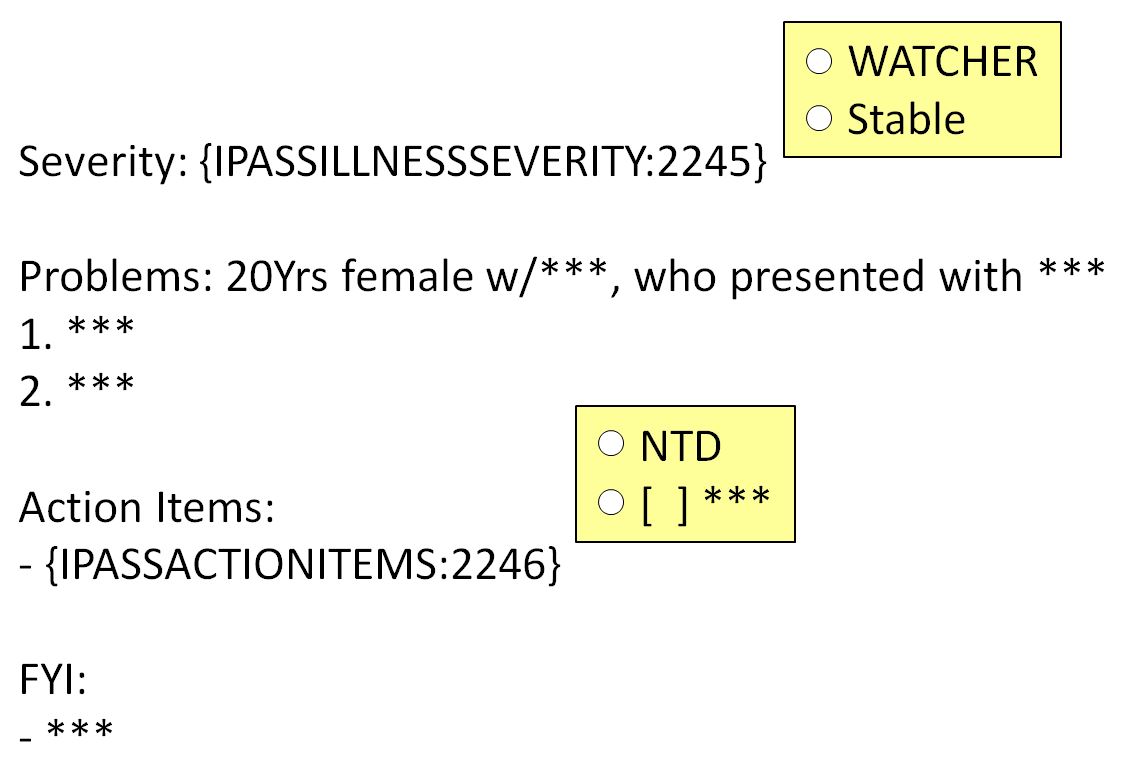
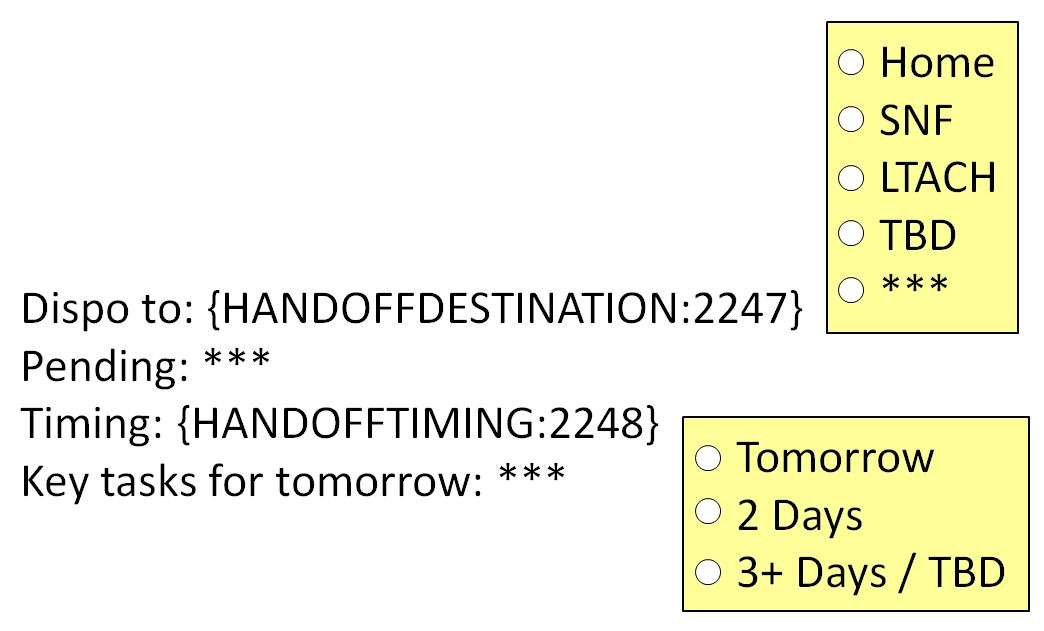
Description: For the past two years, the direct care services of a large hospital medicine group at an urban, academic, tertiary referral center has utilized a modified IPASS template (Figure 1) to facilitate overnight cross-coverage of hospitalist patients. This template uses a standardized approach to highlight severity of illness, key medical problems, action items for a cross-coverage team, as well as any additional pearls for a patient. While our modified IPASS template provides critical information to care for a patient overnight, it lacks the information needed to ensure a seamless end-of-service transition. To solve this problem, we designed an additional template focused on information needed to permanently transition the care of a patient. This end-of-service handoff template (Figure 2) highlights disposition destination, key outstanding hospital issues, timing of discharge, and key tasks for the next day. Taken together, these two templates provide a more complete picture of a patient’s current medical condition as well as key needs for the duration of his or her stay.The new end-of-service handoff template was piloted within a small group of providers, then launched across all hospital medicine services in April of 2019. Its effectiveness has been measured using a pre / post survey looking at time spent preparing end-of-service handoff, additional time spent in the hospital on a provider’s first day of service, and hospitalist confidence in discharge plans received as part of handoff (0 – no confidence to 10 – complete confidence) as well as qualitative interviews. When comparing time spent preparing handoff and additional time spent in the hospital on a provider’s first day of service, no significant differences were seen. Providers did, however, note more confidence in the discharge plans they received from colleagues after the intervention (mean confidence 6.56 vs 5.57, p=0.06). Qualitatively, providers also describe a much easier first day on service in the post-intervention period and report ease in using the new template.
Conclusions: A standardized end-of-service handoff template focusing on discharge disposition, outstanding hospital issues, timing of discharge and key tasks for the following day may improve hospitalists’ confidence in discharge plans as well as ease of practice. Further research should focus on the impact of such interventions on outcome measures including patient safety and length of stay.