Background: Our experience developing the Comprehensive Care Physician (CCP) program within the Section of Hospital Medicine at the University of Chicago has illustrated the value of relational continuity in the care of patients with complex medical needs. For patients with increased risk of hospitalization and who are willing to find a new primary care physician, the program suggests significant value in having a single provider care for patients in both the inpatient and outpatient setting (1,2). Additional opportunities to leverage patient-provider and provider-provider relationships remain for patients at lower risk of hospitalization and those with established primary care relationships.Traditional hospitalist models are based upon schedules where providers work intermittent, intense shifts, typically working 7 days in the hospital followed by 7 days of respite time. These schedules lead to frequent hospitalist-hospitalist handoffs within a patient’s hospitalization. In addition, the large number of hospitalists at many institutions and their intermittent schedules makes it difficult to establish relationships between inpatient and outpatient providers.
Purpose: To better leverage the value of patient-provider continuity within prolonged hospitalizations and provider-provider relationships for hospitalists and outpatient clinicians who frequently admit patients to the hospital, we propose a new model for hospitalist care.
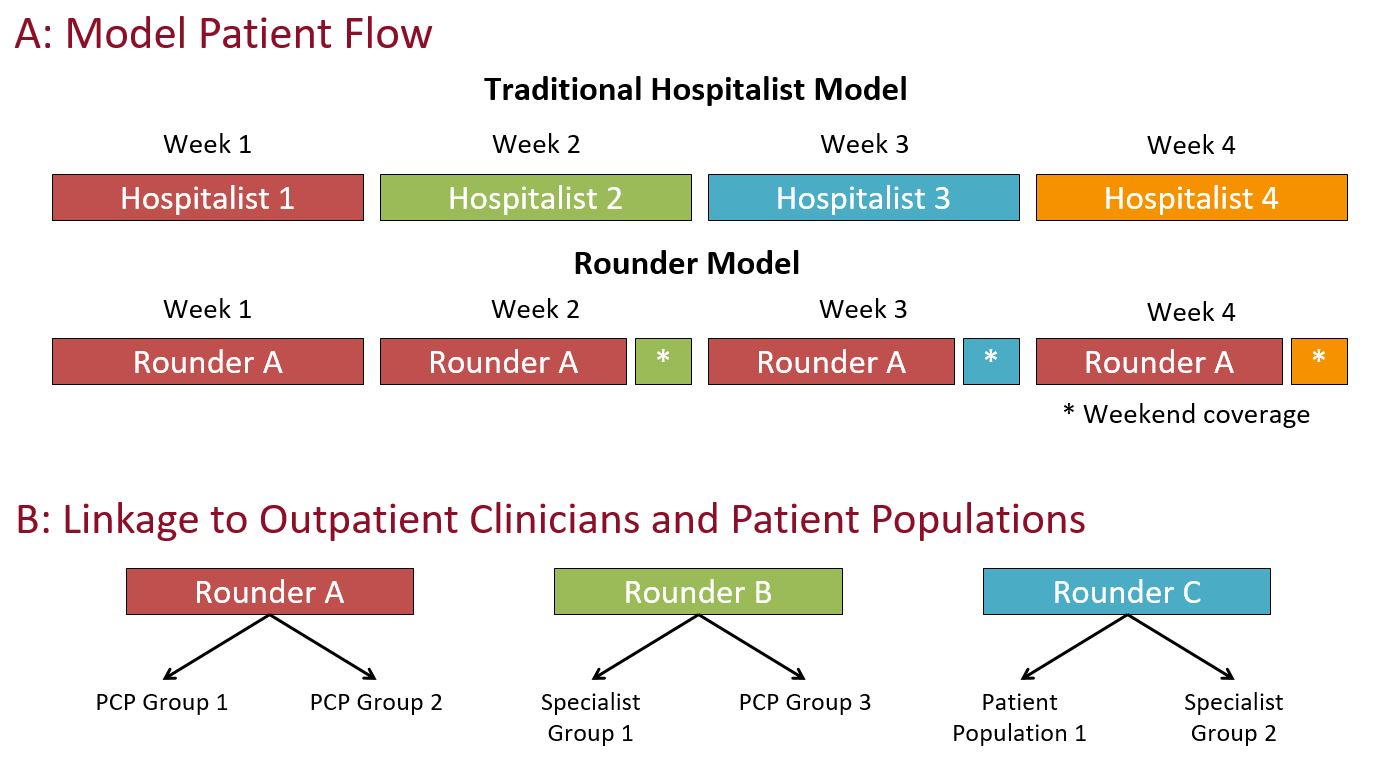
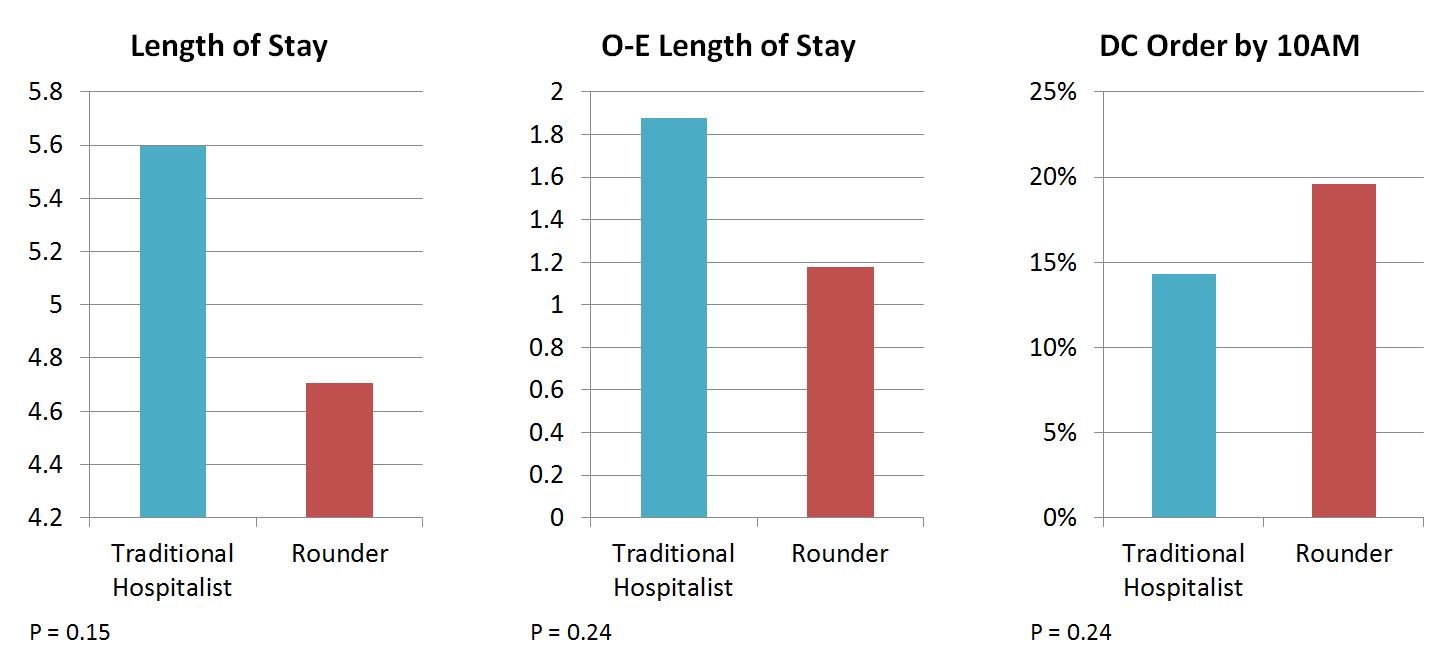
Description: Under the Rounder Model, the work of hospitalists typically performed over intense 7-day periods will be re-allocated across more weekdays, thereby enabling hospitalists to sustainably work more days per year. This reorganization of hospitalist work will enable greater patient-provider continuity within hospitalizations by enabling individual hospitalists to direct the care of a patient throughout his or her entire hospitalization (Figure 1A). The Rounder Model will also enable pairing of individual hospitalists or small groups of hospitalists to outpatient providers to promote provider-provider relationships across the inpatient and outpatient domain as well as patient-hospitalist relationships for patients from paired groups who are frequently hospitalized themselves (Figure 1B).To-date, the Rounder Model has undergone a four-week pilot with four providers within the Section of Hospital Medicine at the University of Chicago. Though not powered to show significance, data from the pilot suggests the potential or the model to improve efficiency metrics including length of stay, observed-expected (O-E) length of stay, and early entry of discharge orders (Figure 2). Initial feedback has shown significant satisfaction by participating hospitalists who describe significantly greater control over patient plans as well as a greater degree of work-life balance and sustainability. In addition, physicians described an increased sense of trust, collaboration and accountability within the small team working together. The broader multidisciplinary care team also noted stronger relationships between nurses, case managers, social workers, and physicians during the pilot period.
Conclusions: Redesigning hospitalist service structures may offer a sustainable opportunity to improve continuity of care. Evaluation of future model iterations will focus on establishing the impact of this novel operational model on additional outcome measures including patient and provider satisfaction, quality measures, and length of stay.