Background: Although the vast majority of adult patients in the United States prefer to die at home, most patients die in acute care settings. Barriers include advanced care planning, communication between inpatient and outpatient providers, and delivery of medical equipment. In 2018, our General Medicine Service Line ranked 73rd out of 98 Academic Medical Centers for inpatient mortality. A retrospective chart review of all patient deaths that occurred during this period showed that most patients were 80+ years old and 80% with at least one hospitalization in the past month. Almost 3/4 of these patients were critically ill at the time of their presentation to the Emergency Room with 1/4 of patients passing away within 48 hours of admission. These cases accounted for the majority of inpatient mortality on our inpatient general medicine service.
Purpose: As health care providers, it is our responsibility to understand patient wishes at the end of life and have the systems and processes in place to fulfill their needs. The purpose of this multidisciplinary/inter-departmental initiative was to improve advanced care planning, communication between medical providers, and mobilization of resources and support for patients at the end of life. We hoped this would decrease readmissions and unnecessary hospital admission at the end of life, thus improving our ability to carry out patient wishes while reducing overall mortality
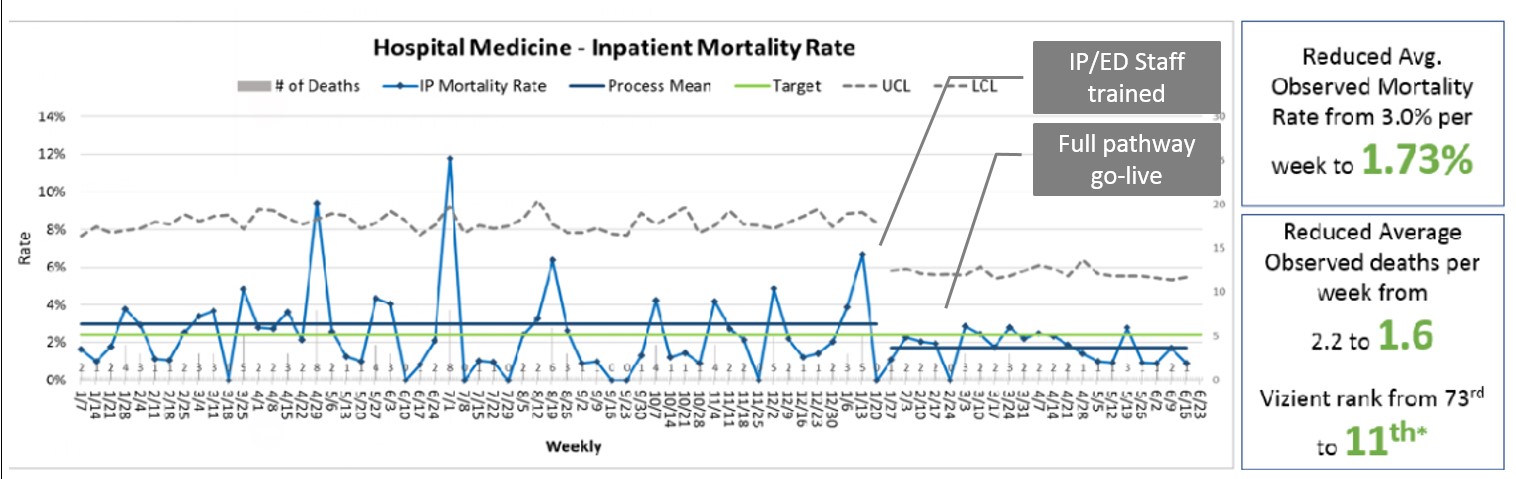
Description: In early 2019, we convened an interdisciplinary workgroup from Hospital Medicine, Emergency Medicine, and Palliative Care. Multiple pathways were developed while streamlining and integrating existing workflows in the following domains: Advanced Care Planning: a) Identification of patients with high risk for mortality and readmission, b) Education and orientation of housestaff regarding goals of care discussions and completion of POLST forms prior to discharge. Communication: a) Contacting outpatient providers and sub-specialists to clarify prior and ongoing goals of care conversations, b) Development of an EHR-based notification (“flag”) to alert Emergency Room triage staff of previously identified high-risk patients. Support: a) Early consultation of geriatrics and/or palliative care services, b) Early engagement of case managers and social workers, b) Emergency Room-based pathway to mobilize resources including physicians, palliative care, social work, and case managers, c) Weekly review of all inpatient mortality cases with survey feedback from primary team to identify systems opportunities and unforeseen patient needs. Most “flagged” patients were discharged without subsequent 30-day representation to the ER. After implementation of our intervention, observed deaths decreased from 2.2 to 1.6 per week. This reduced the observed mortality from 3.0% per week to 1.7% per week, representing a 41.3% decrease. Discharges to hospice per inpatient hospital death also improved to from 1.3 to 2.0 during the intervention period. Inpatient mortality compared with peer academic institutions subsequently improved from 73rd to 11th.
Conclusions: Multi-disciplinary and interdepartmental approach to end of life care can improve our ability to not only understand patient wishes and goals of care, but also successfully carry out their plan. As patients are often admitted to hospital medicine services when other specialties have little to offer, additional upstream discharge and readmission pathways should also be considered in the future in conjunction with other departments.