Background: Using evidence-based clinical pathways has been shown to improve mortality in patients with staphylococcus aureus bacteremia. However, little is known if these pathways can decrease antibiotic use as a means of antibiotic stewardship in patients with suspected contaminated blood cultures.
Purpose: We aim to decrease antibiotic use in clinically stable patients with likely gram-positive cocci (GPC) contaminated blood cultures by deployment of a GPC bacteremia pathway.
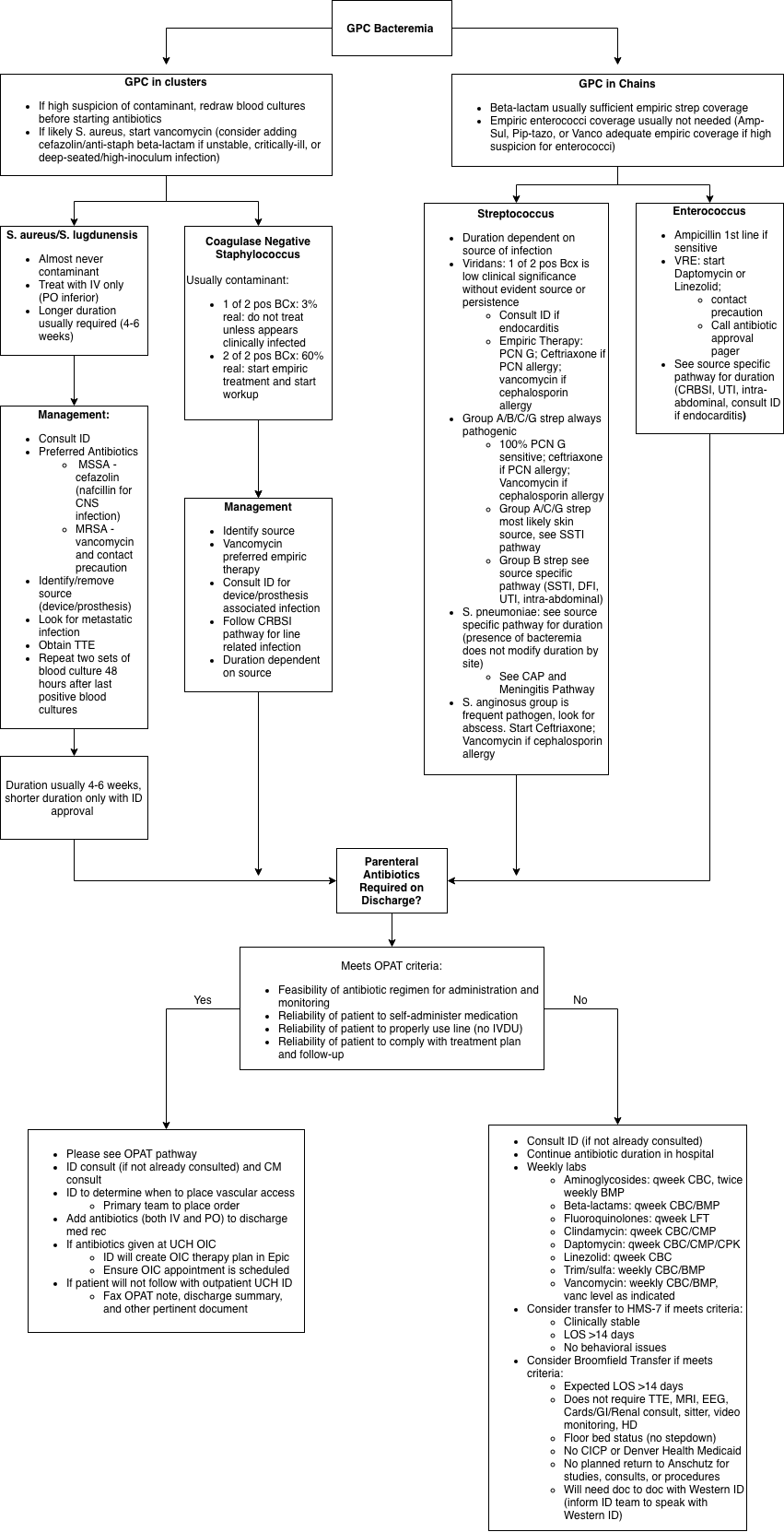
Description: A group consisting of hospitalists, infectious disease physicians, and an infectious disease pharmacist designed a clinical pathway to guide the inpatient internal medicine teams on choosing the correct initial empiric antibiotics for patients with GPC blood cultures. As part of the pathway, antibiotics were to be held in patients who are clinically stable and have positive GPC blood cultures suspicious for contamination.
The pathway will be built into the electronic medical record at the University of Colorado Hospital and will be implemented in December 2018. Baseline data were obtained between June 2018 and November 2018 that looked at the length of stay, mortality, and antibiotic use in all medicine patients in the non-critical care units who had blood cultures growing common contaminants such as coagulase-negative staphylococcus, not lugdunensis and staphylococcus epidermidis. Baseline data showed 65 patients admitted met these criteria. The average length of stay was 6.89 days with no in-hospital deaths. Fifty-one percent of these patients were started on antibiotics or had antibiotics continued at the time of the first positive blood cultures despite clinical stability. Data will continue to be collected on a monthly basis after implementation of the pathway.
Conclusions: Appropriately decreasing antibiotic use in patients is an important part of antibiotic stewardship. Implementing a clinical pathway for GPC bacteremia may limit inappropriate use of antibiotics in the hospital.