Background: Secure text messaging platforms are increasingly replacing traditional paging systems for in-hospital communication1,2. At our institution, the number of secure texts per month nearly doubled from 4.4 million in September 2020 to 8.1 million in September 2023. This growing burden of automated notifications from secure texts without a framework to triage message urgency contributes to alert fatigue, workflow interruptions, and increased task switching, which in turn may result in clinician burnout or medical errors3.
Purpose: In this single-site quality improvement study utilizing A3 methodology, we piloted an intervention aimed at reducing interruptions and alert fatigue from secure texts by leveraging native functionality to designate message priority and suppress non-urgent messages.
Description: Twenty-six hospitalists (physicians and APPs) working at a university-affiliated community hospital participated in the intervention between February 20, 2024 and April 1, 2024. During the intervention period, the hospitalists were asked to set their “Presence” to “Busy” on the secure texting platform (Voalte Inc.) for the entirety of their shifts. While in the “Busy” presence, only messages marked by the sender as “Urgent” priority trigger an audible notification; messages with “Regular” priority are delivered silently with a vibration only. Education was provided to clinicians and multidisciplinary teams before pilot initiation and at regular intervals through e-mail communication, division or team meetings, and in-person rounds. The primary outcome was hospitalist-reported number of interruptions attributed to non-urgent secure texts. Process and balancing measures included utilization of Busy presence, number of audible notifications generated, time to read messages, and safety events. The baseline period was defined as December 1, 2023 and February 19, 2024. Pre- and post-pilot surveys and secure text usage data were collected.
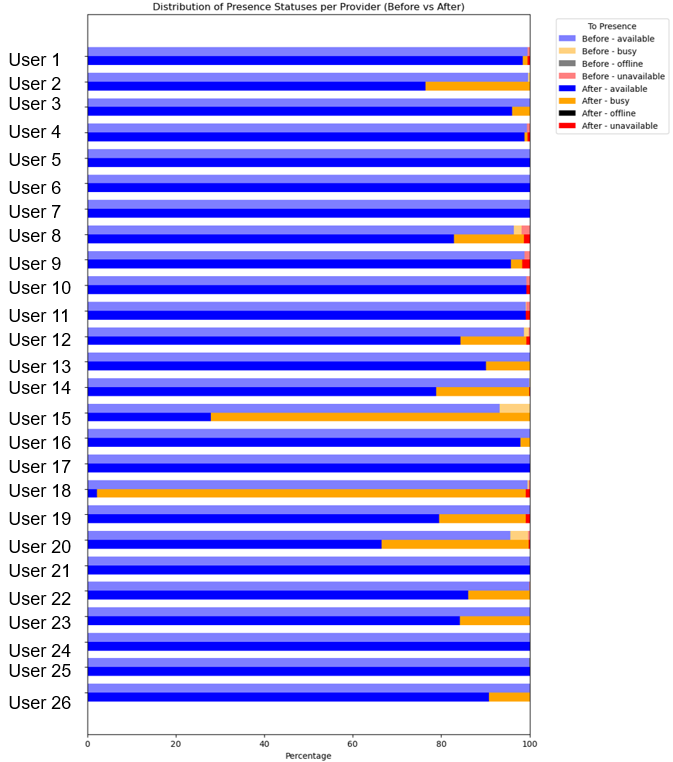
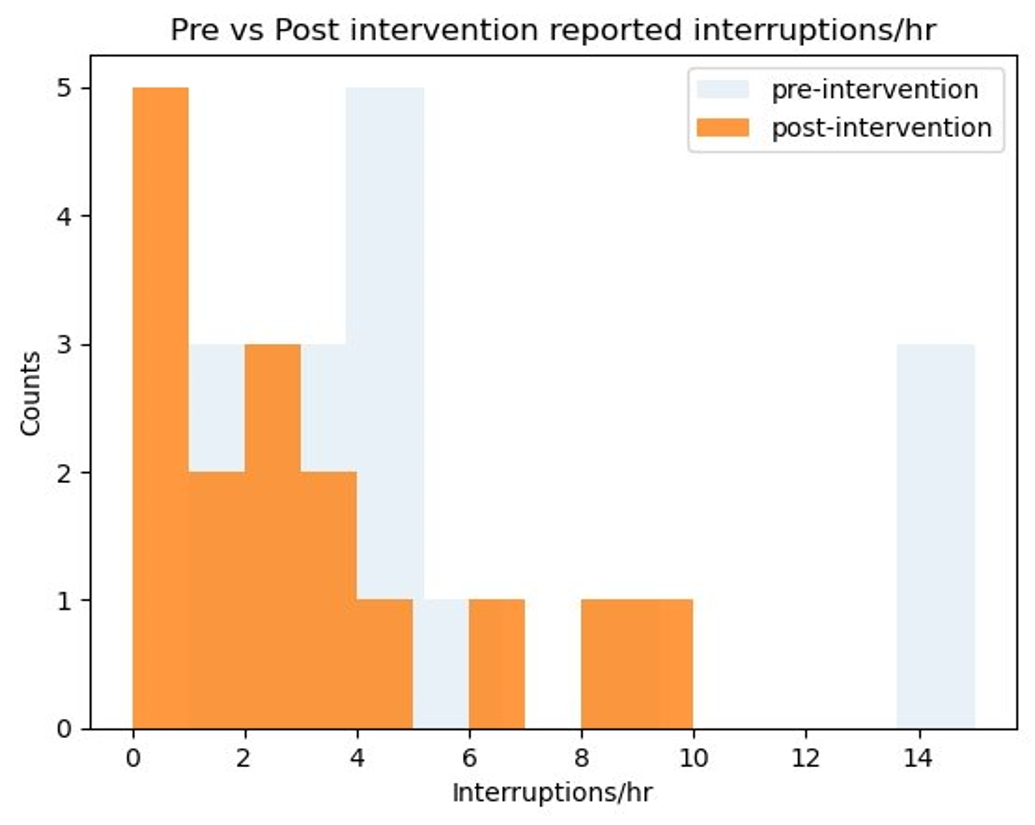
Conclusions: Pilot users received on average 19.1 messages/user/day during both baseline and pilot periods. Users logged in as Busy significantly more during the pilot (0.58% vs 13.6%), but utilization varied widely (Fig 1). Silently delivered messages increased significantly from 0.56% to 13.4% of all received messages, or 0.1 to 2.5 silent deliveries/user/day. There was no significant change in time to read messages or reported safety events during the intervention period. Hospitalist-reported average interruptions/hour reduced significantly from 6.1 to 2.6 (57.3%) following intervention (Fig 2), and surveyed users felt improvement in the secure text experience. Limitations included small sample size, variable intervention uptake, and recall bias. Native functionalities of secure texting platforms can be leveraged to effectively reduce interruptions from audible notifications in the hospital. This “Busy” strategy has potential to mitigate alert fatigue and clinician burnout without significant adverse effects.