Background: The ABIM’s Choosing Wisely campaign targets daily phlebotomy in medical inpatients as an area of potential wasteful care. Unnecessary phlebotomy increases labor and costs while negatively impacting patient’s through hospital-acquired anemia, intravenous access issues, and false-positive results. While previous interventions have attempted to reduce overall labs ordered, few studies have examined educational attempts to reduce unnecessary lab orders.
Purpose: Using LEAN methodology, we identified underlying causes of unnecessary phlebotomy on an inpatient internal medicine teaching service and implemented a solution to reduce waste. Our primary goal was to reduce the number of unnecessary labs ordered by 50 percent. As a secondary goal we aimed to reduce the total number of labs per patient admission.
Description:
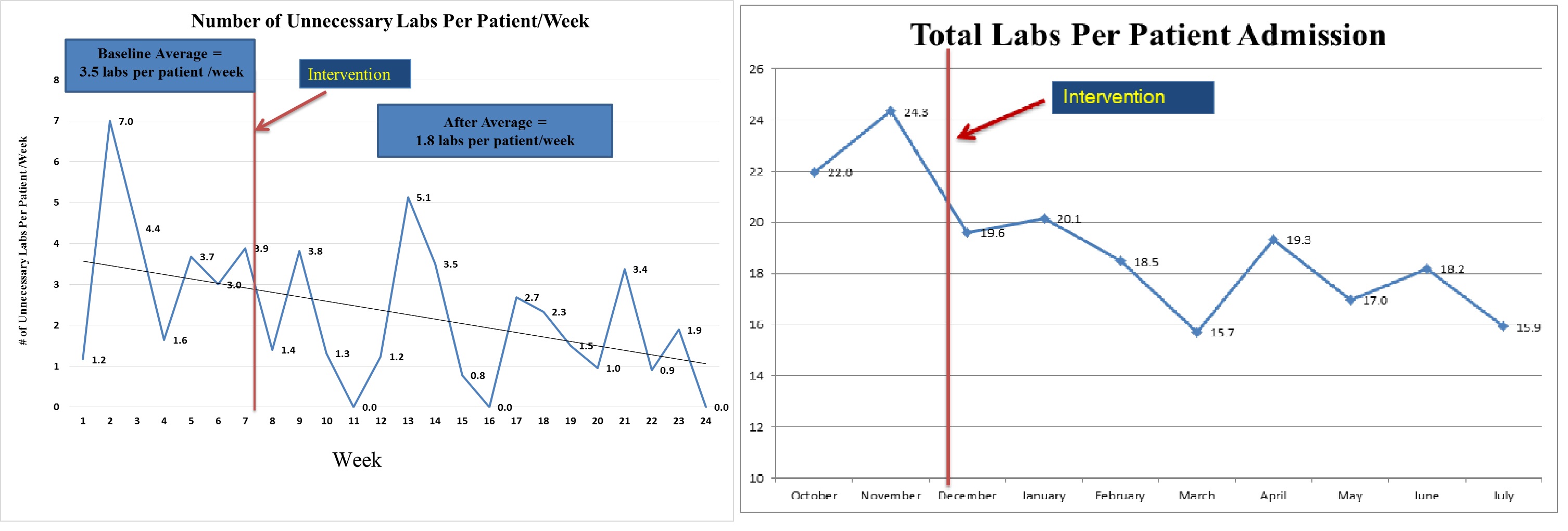
Attending physicians sampled lab orders one day per week over a 6 month period to determine whether a lab was unnecessary. A lab was considered unnecessary if two attending physicians rated the lab as unnecessary. Attendings based their decision on the following statement: “An unnecessary lab is one that is not used for diagnosis, treatment decisions or treatment monitoring”. Baseline data demonstrated that an average of 3.5 unnecessary labs were ordered per patient per week.
Focus groups with housestaff identified that many labs are ordered out of fear of missing abnormal results and for provider reassurance, rather than for medical necessity. Based on these findings, we implemented two strategies to reduce unnecessary lab orders:
1) Attending consensus guidelines for indications for common labs were added to the lab ordering menu in the electronic medical record and displayed prominently in resident work rooms.
2) Attending feedback was given to teams on thier lab orders once per week using a standardized checklist.
We conducted a pre and post intervention analysis of data which showed a 46% reduction (p=0.054) in unnecessary labs from baseline of 3.5 to 1.9 per patient per week (Figure 1). The monthly total number of labs ordered per patient admission also fell from 23.1 to 18.0, a 22% reduction (p<0.05 )(Figure 2).
Conclusions: We were able to reduce both the number of unnecessary daily labs as well as average total labs ordered per patient admission through a combination of educational guidelines and attending feedback. Our approach focused on interventions that reassured house staff that they can omit labs when not medically indicated. Other institutions could consider implementing these strategies to improve patient care quality and reduce waste in their hospitals.