Background: Hospital discharge is a complex process that requires coordination from various parties. There still remains a significant rate of readmission, with a reported 30 day readmission of roughly 20% and annual cost of $18 Billion to Medicare. Patients with adequate discharge planning have a decreased readmission rate. Recent studies that demonstrated that high risk patients should receive follow-up within 7 days. Patients hospitalized for COPD have a 20% readmission rate and account for the third most common cause of rehospitalization.
Methods: The Integrated Michigan Patient-Centered Alliance in Care Transitions (I-MPACT) is a grant-funded, patient-centered Collaborative Quality Initiative. The collaborative is composed of numerous “clusters”, each of which is comprised of a hospital organization, provider organizations, and patient/caregiver teams. Each cluster selects one patient population from four designated disease states to implement interventions aimed at improving care transitions. We specifically studied COPD patients who received at least the “7-Day follow-up” intervention. For this intervention, appointments were made with either established Primary Care Physician, Pulmonologist, or other physician, and were scheduled for 5-7 days from discharge. We used a sample of 898 COPD patients discharged from five hospital sites between October 2017 and June 2019 and recorded readmission within 30 days of discharge. Stepwise logistic regression was used to select adjusted models using 28 demographic, transition of care, and clinical covariates.
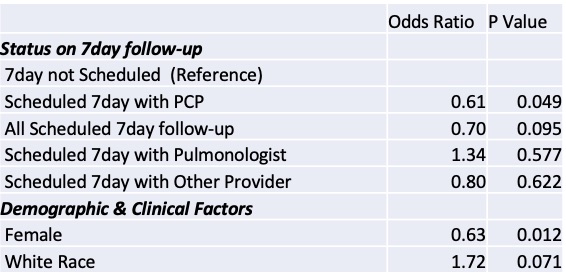
Results: Mean age of the sample was 67 years. The sample was 57% female, 75% white, and 12% on Medicaid. 28.8% of patients had a scheduled follow-up appointment; 21.8% of patients with a PCP, 2.5% with a pulmonologist, and 4.6% with a provider other than a PCP or pulmonologist. Scheduling with a PCP was associated with decreased probability of readmission than not scheduling an appointment (14.8% vs. 18.8%, OR=0.61, P=0.05) while scheduling with a pulmonologist was associated with increased risk of readmission than not scheduling an appointment (27.3% vs. 17.7%, OR=1.33, P=0.58). Scheduling with a provider other than a PCP or pulmonologist had little effect on readmission compared to not scheduling an appointment (17.1% vs. 17.9%, OR=0.8 P=0.62). Readmission rate among patients receiving any 7day was 16.2% while rate among patients not receiving a 7day was 18.6% (OR=0.70, P=0.095).
Conclusions: Our study indicates that 7-Day follow-up with an assigned PCP has a statistically significant protective effect on readmission for patients hospitalized with COPD. We anticipate that this effect will likely be replicated in other disease states studied in the QI Initiative, proving a generalizable benefit of close PCP follow-up after hospitalization. Further study will need to be done into the effect of follow-up with pulmonologists and other physicians, as this data was not statistically significant.