Background: The most recent guidelines regarding telemetry monitoring use and indications was published by the American Heart Association (AHA) in 2017.(1) However, most institutions lack evidence-based protocols to guide telemetry usage which could improve overuse. Telemetry monitoring overuse in non-critical patients has been recognized as a contributing factor to healthcare cost, length of stay and staff dissatisfaction. An example in a single institute showed that incorporating AHA guidelines into an electronic medical record (EMR) system and nursing driven discontinuation protocol resulted in a sustained reduction in the number of unnecessary telemetry orders while adverse events rates remained stable.(2) At our institution, telemetry monitoring overutilization has been recognized as a source of inefficiency of throughput, increased length of stay and ED holds for admitted patients. Given the large percentage of telemetry admission orders that were not supported by current guidelines, a resident-led QI initiative was undertaken to address this institutional priority.
Methods: We collected pre-intervention data including all patients (n=515) who were on telemetry monitoring between 6/3 and 7/6/2018. We developed a guideline-driven telemetry monitoring protocol and analyzed the characteristics of the data, which included an appropriateness of telemetry monitoring orders by each provider groups. Based on the analysis, we decided to target ED and resident physicians. By creating a 2-by-2 impact-effort matrix, two main interventions were implemented — creation of EMR telemetry order set incorporating the guideline-driven protocol, and targeted education to high-yield groups by using sample clinical scenarios. Other interventions included best practice alert (BPA), embedding the telemetry order set in the admission order sets, and discontinuation of the ED telemetry orders to wards.
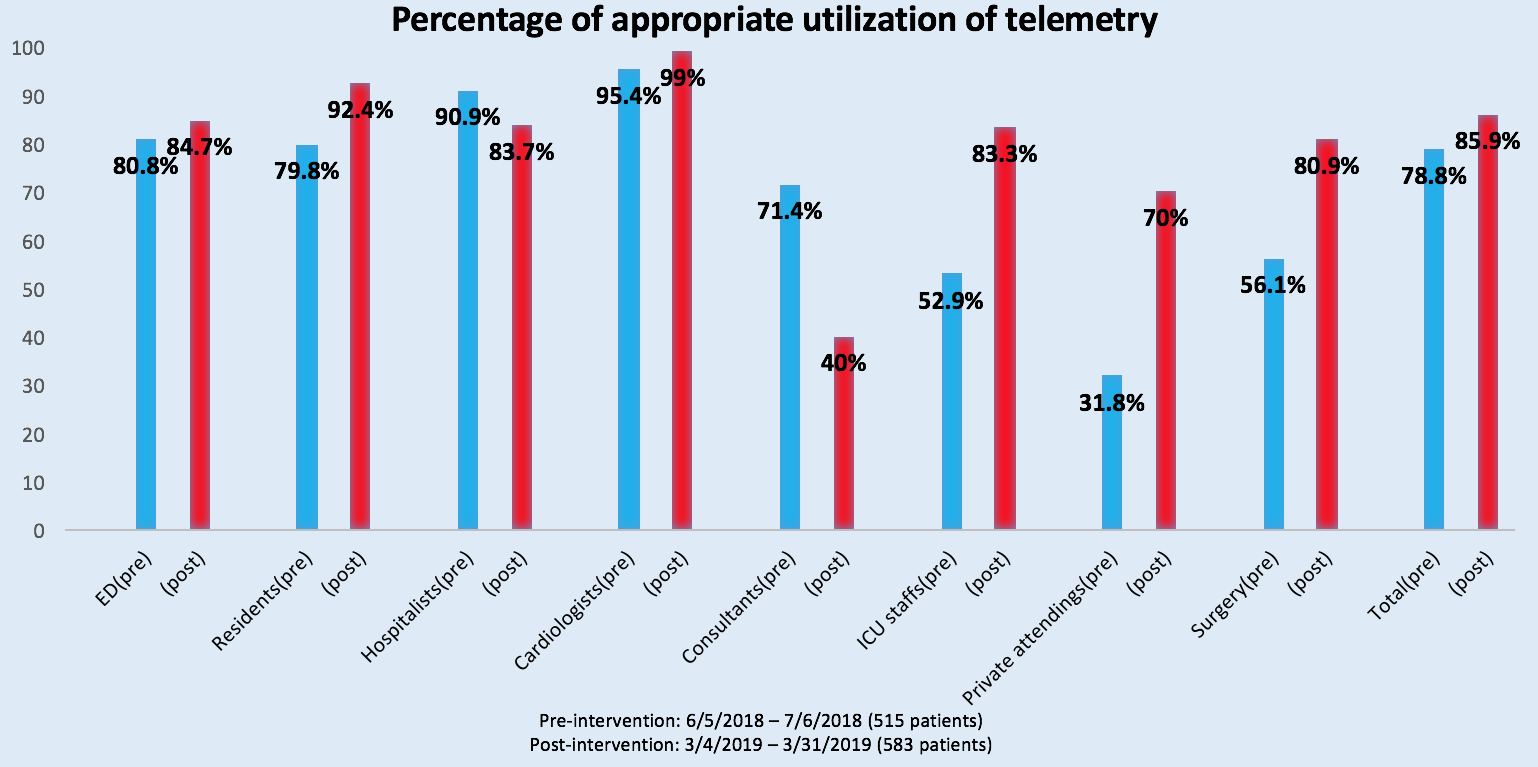
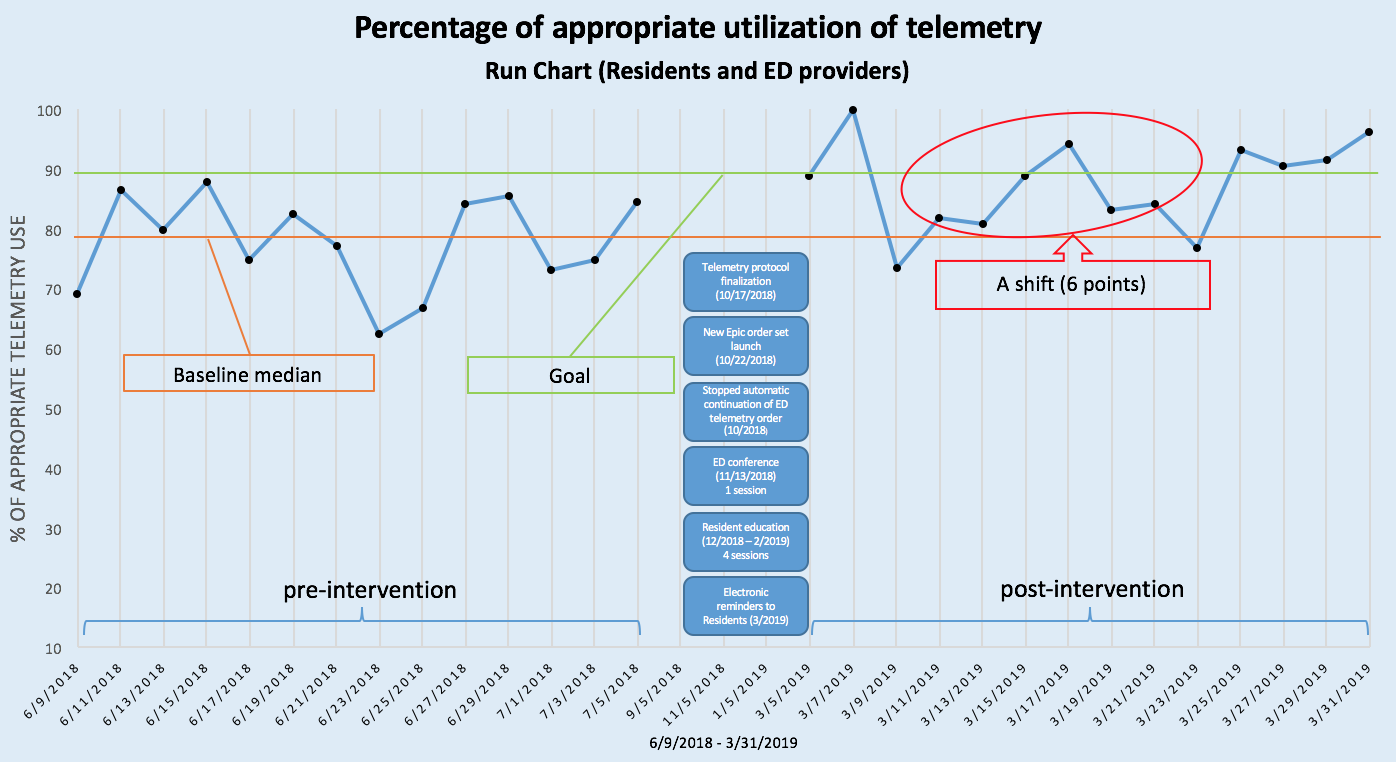
Results: After these interventions, post-intervention data was collected, including all patients (n=583) who were on telemetry monitoring between 3/4 and 3/31/2019. Patients’ data were thoroughly reviewed and assessed based on the protocol. Three resident physicians assessed the appropriateness and resolved disagreements through discussion. ED physicians showed improved appropriateness to 84.7% from 80.8%, and resident physicians showed improved appropriateness to 92.4% from 79.8%. The remainder of provider groups also showed improvements and the overall ratio improved to 85.9% from 78.8%, highlighting that the EMR telemetry order affected all provider groups (Figure 1). A run chart methodology was utilized to evaluate a non-random pattern that can signal an improvement. With baseline median (78.65%) from the pre-intervention data, a shift (6 consecutive points above the median) was identified. The number of runs (12) were within an upper and lower limits, signaling a random pattern (Figure 2).
Conclusions: Creating a guideline-driven EMR telemetry order set and targeted educational program by using common clinical scenarios can effectively decrease unnecessary utilization of telemetry monitoring in a short term. Limitations of our study are, challenges of education-based intervention and addressing only a “Front-end” aspect of telemetry monitoring overutilization. Future QI projects targeting a “Back-end” aspect of the overutilization by implementing a nurse driven protocol to safely discontinue telemetry after 48 hours is planned.