Background: Studies have reported an association of physician burnout with lower patient satisfaction and poor quality of health care. Hospitalists play a large role in inpatient care, however, to the best of our knowledge only one study has examined the association of hospitalist burnout on patient satisfaction but found no significant association. Therefore, the objective of this study was to examine the relationship between hospitalist burnout and patient satisfaction.
Methods: We conducted a cross-sectional survey of patients admitted to the hospital medicine service at a large, quaternary care academic hospital. The survey collected demographic data on patient’s age, race, and gender using two patient satisfaction questionnaires: 1) the Tool to Assess Inpatient Satisfaction with Care from Hospitalists (TAISCH), and 2) the 5-question satisfaction (5QS) tool. Patients were enrolled if they were cared for by the same hospitalist provider for at least 2 consecutive days. To measure hospitalist burnout, we also surveyed hospitalists with the Oldenburg Burnout Inventory (OLBI), a validated tool to assess burnout and workplace engagement. OLBI measures burnout on a 4-point Likert scale. Burnout was defined as the presence of both exhaustion and disengagement above 2.25 and 2.10, respectively. Surveys were administered from April 2018 until October 2018. Descriptive data was collected from providers including age, gender, and year(s) since graduation. To account for correlation induced by observation from the same physician, we used mixed linear effects models to examine the relationship between patient satisfaction and physician burnout.
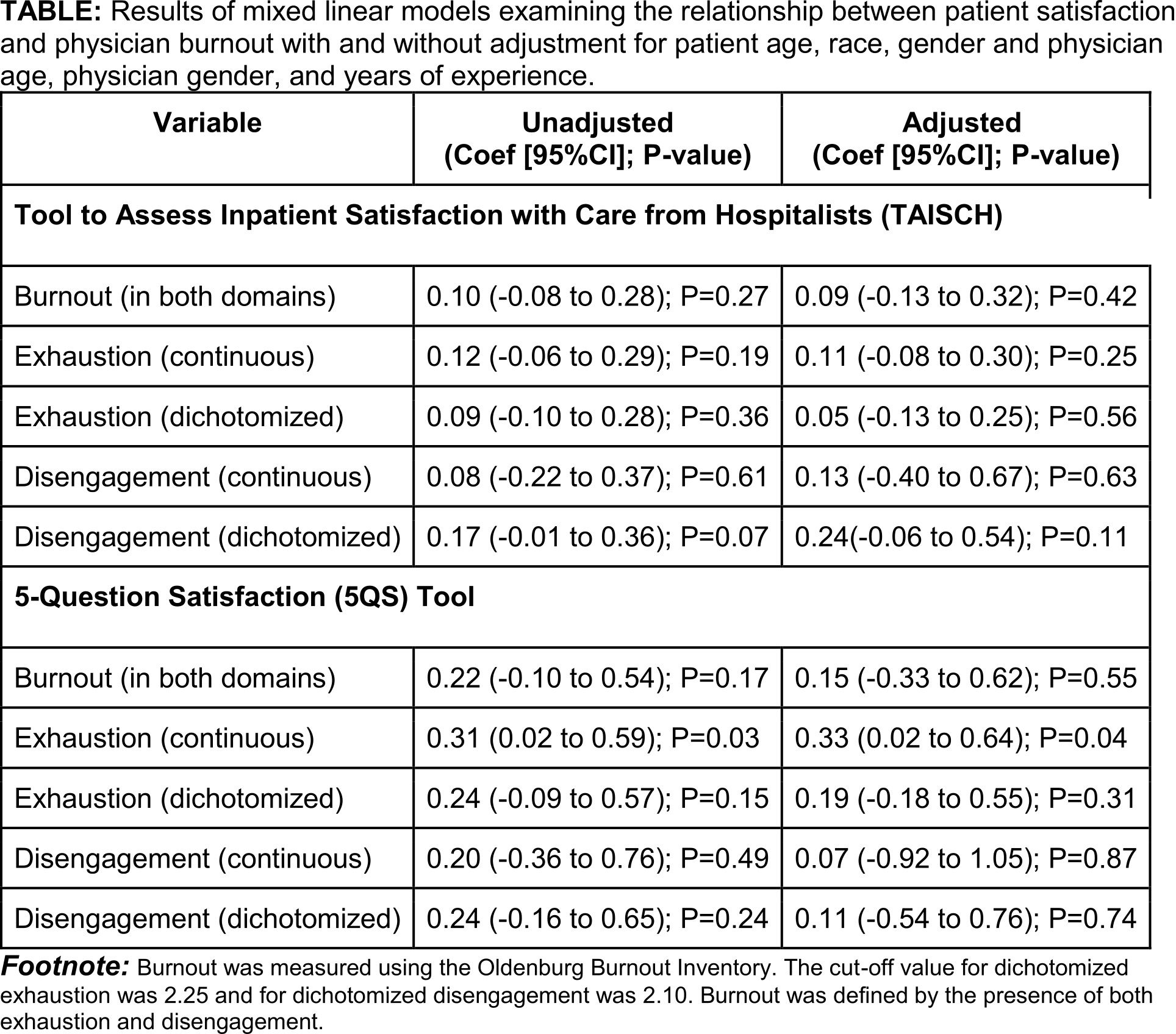
Results: Of the 137 patients who participated in the study, 71(52%) were females, 80(58%) were African Americans, and had a mean(SD) age of 53.8(6.0) years. Mean(SD) satisfaction scores were 3.8(0.3) and 9.1(0.6) on TAISCH and 5QS, respectively. Thirty-seven (63%) of the 58 physicians agreed to participate in the study (mean (SD) age = 36.1[5.9] years, females = 19[51%]). Burnout was present in 18(49%) physicians and prevalence was higher in females (72% vs. 28%; P = 0.01). There was no difference between hospitalists with and without burnout in patient satisfaction as measured by TAISCH (3.9 vs 3.7; P = 0.14) or by 5QS (9.3 vs. 8.9; P = 0.08). In unadjusted and adjusted mixed linear models, there was no relationship between patient satisfaction and burnout or individual domains of burnout with one exception; each one unit increase in exhaustion was associated with a 0.33 units increase in patient satisfaction as measured by 5QS (Table).
Conclusions: We did not find an association between patient satisfaction and physician burnout except that physicians with a higher level of exhaustion were more likely to have higher patient satisfaction. It is possible that the greater amount of work that leads to physician exhaustion is also associated with higher patient satisfaction, however, this hypothesis needs further study.