Background: The SARS-CoV-2 (COVID-19) outbreak is rapidly spreading worldwide and as a result clinical predictors of disease severity are critical for appropriate management and disposition of patients. An early and accurate risk stratification of COVID-19 patients may have a great impact on their prognosis given rapid patient deterioration and continued need for rationing of treatments. Dysnatremia has previously been identified as an independent risk factor for mortality and increased length of stay in hospitalized patients, specifically in patients with community acquired pneumonia [1,2,3,4], however, its relevance in COVID-19 patients has not been reported. This study aims to describe the prevalence of dysnatremias in COVID-19 cases and to evaluate its impact on mortality.
Methods: All adult COVID-19 patients admitted to our tertiary care academic medical center from March 13th to September 13th, 2020 were included in the study. Demographic, clinical, and laboratory data were collected from electronic health records. Daily serum sodium levels were categorized into 140 mEq/L. Mean (SD) or frequencies were used as appropriate to summarize data. Primary outcome was death during hospitalization or discharge to hospice. We used Cox proportional hazards models to examine the relationship between the primary outcome and serum sodium with sodium as time-varying variable. Time to event was noted from arrival to hospital to discharge from hospital or the primary outcome. To determine when, during hospitalization, serum sodium levels become predictive, we used logistic regression models to examine the relationship between primary outcome and serum sodium on day#1, day#4, and day#10 from admission. Models were adjusted for age, race, gender, and BMI.
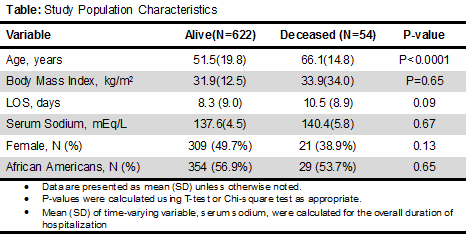
Results: Of the 676 patients included in the study, 54 (8%) met primary outcome (died during hospitalization or discharged to hospice), 330 (49%) were females, 383 (57%) were blacks, with a mean age of 52.7 (4.5) years and BMI of 32.1 (15.5) kg/m2 (Table). Mean serum sodium was 137.9 (4.8) mEq/L with between-person SD=3.7 and within-person SD of 3.0. On an average, a person had serum sodium 140 during 55.9% of the hospitalization days; 81.2% of the patients had a least one day with sodium >140. In unadjusted models, each 1 mEq/L increase in serum sodium was associated with 11 % increase in hazards of primary outcome (HR =1.11 95%CI=1.05, 1.15; P<0.001) which did not change after adjustment for potential confounders (HR=1.11, 95%CI=1.05, 1.16;P<0.001). Serum sodium level >140mEq/L was associated with 2.7 times higher risk of primary outcome (adjusted HR=2.67, 95%CI=1.53, 4.66; P=0.001). Admission day serum sodium were not associated with primary outcome but serum sodium level >140 mEq/L were associated with higher risk of outcome on day#4 (adjusted OR=2.4, 95%I=1.2, 4.5, P=0.008) and day#10 (adjusted OR =5.3, 95%CI=2.1, 13.2; P<0.001).
Conclusions: We report a novel finding of a relationship between mortality and serum sodium that is apparent early during hospitalization. Further, we show that the relationship remains stable after adjusting for confounders. The underlying reason for this association remains unclear and needs further study.