Case Presentation: IntroductionHistoplasmosis is a fungal infection caused by histoplasma capsulatum, a dimorphic fungus endemic in central and eastern United States. Even in immunocompromised patients, the reported incidence of CNS manifestations in disseminated histoplasmosis is only about 5-10%. This report presents an unusual case of recurrent histoplasma meningitis in a patient with prior history of disseminated histoplasmosis.
Clinical case
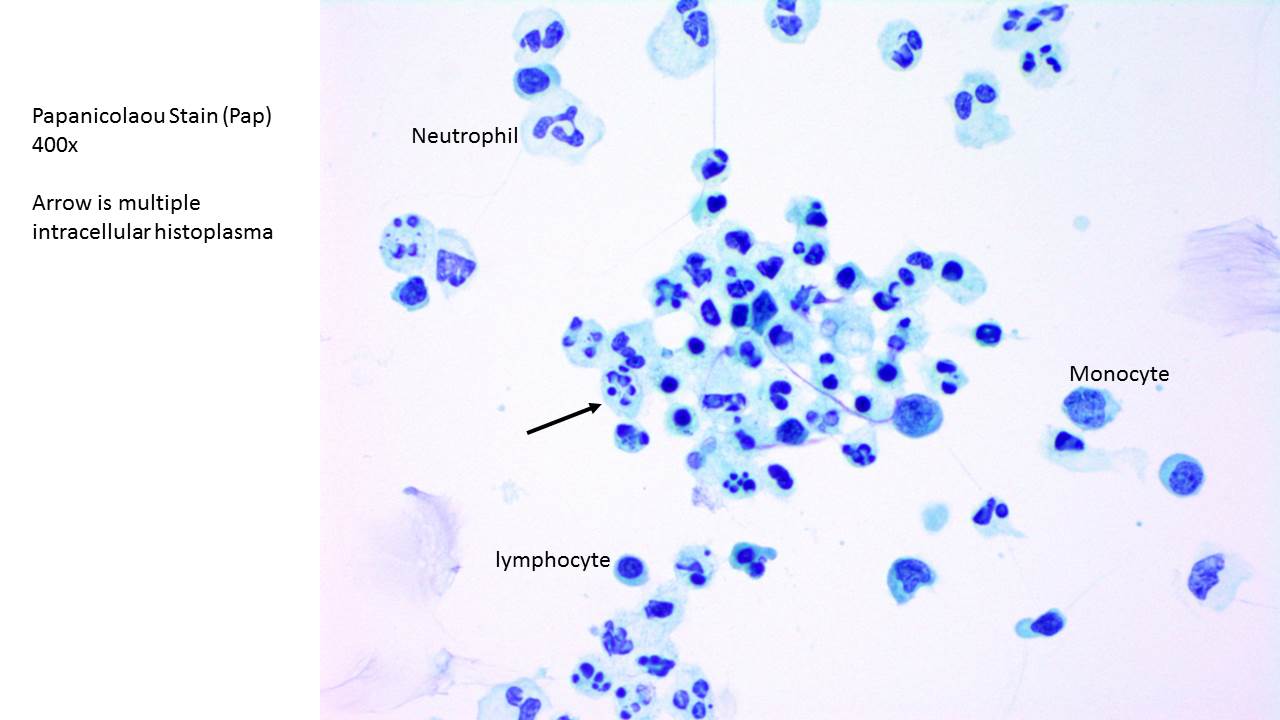
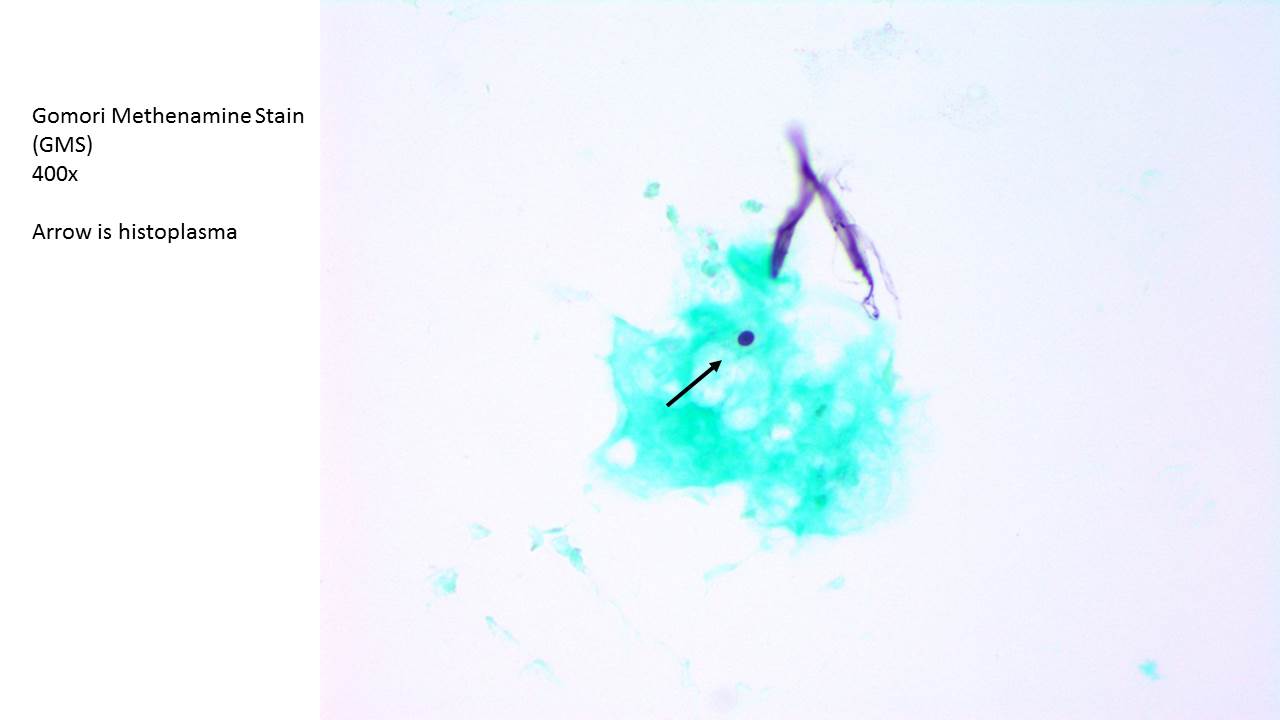
A 41 year old African American male with past medical history significant for HIV/AIDS (CD4 absolute count of 1 ) non-compliant with anti-retroviral therapy, prior history of disseminated histoplasmosis with histoplasma meningitis , suspected cerebral toxoplasmosis, presented with altered mental status. The patient was obtunded and intubated for airway protection. The patient was started on broad-spectrum antibiotics, antivirals, and antifungal coverage with liposomal amphotericin B given concerns for bacterial meningitis, as well as opportunistic infections including recurrent histoplasmosis. CT head on admission showed no acute intracranial abnormalities, and subsequent MRI without contrast was also unrevealing. CSF analysis was significant for a white blood cell count of 465/CMM with lymphocytic predominance , red blood cells of 0/CMM, non-quantifiable amounts of protein and thus reported as greater than 200 mg/dl, and glucose less than 15 mg/dl.
Urine histoplasma antigen was positive at 1.59 ng/mL (reference range more than 0.4 ng/ml considered positive). CSF cultures were positive for Histoplasma capsulatum. Additional CSF testing was negative for HSV PCR, cryptococcal antigen and TB PCR. At this point, empiric antimicrobial therapy was de-escalated to Liposomal Amphotericin B. Patient was noted to have gradual improvement in mental status and was successfully extubated on hospital day 14. On hospital day 18, a repeat CSF analysis showed significant improvement in cell counts: white blood cell of 27/CMM, now quantifiable amounts of protein at 529 mg/dl, and glucose of 64 mg/dl. Patient was subsequently switched from liposomal amphotericin to itraconazole on day 18 and discharged to a long-term acute care facility.
Discussion: There are other case reports of histoplasma meningitis, mainly in endemic areas such as Texas. However outcomes are usually very poor. This case of recurrence is unusual, given the high mortality of this disease after a single infection.
This case was not unusual in terms of initial presentation and nor different from standard guidelines of treatment either, despite the fact that patient was non-compliant, which in theory could have increased his risk of resistance to drugs. However this patient had an unusually good clinical outcome which may be due in part to the prompt initiation of empiric therapy for suspected histoplasmosis.
Conclusions: This case highlights the importance of considering histoplasmosis in immunocompromised patients with appropriate epidemiologic background and the prompt initiation of therapy for histoplasmosis while the diagnostic work-up is underway to try to achieve improved outcomes.