Case Presentation: A 34-year-old man with history of injection (IV) heroin misuse, anxiety, and homelessness presents with dyspnea and pleuritic chest pain. He was recently hospitalized with Methicillin-Sensitive Staph Aureus (MSSA) tricuspid valve (TV) endocarditis complicated by acute heart failure and septic pulmonary emboli but left against medical advice.
On admission he was afebrile, tachycardic to 130s and hypertensive to 167/87 with normal respiratory rate and pulse oximetry. Physical exam revealed a pansystolic murmur, S3, jugular venous pressure to 11cm, diffuse pulmonary crackles, and 2mm of bilateral pitting edema up to mid-calf.
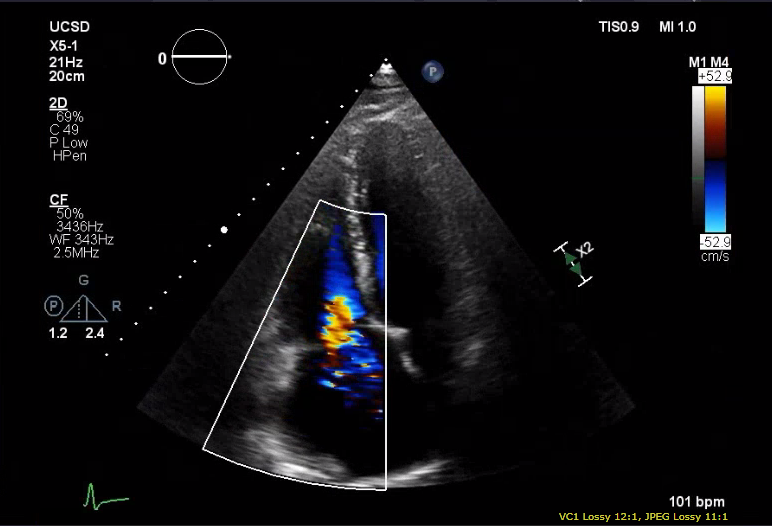
Labs were notable for leukocytosis of 16.3 and BNPP>7000. EKG noted sinus tachycardia with left atrial enlargement. CT chest demonstrated bilateral septic pulmonary emboli and cavitary nodules. Transthoracic echocardiogram identified a TV vegetation, severe tricuspid regurgitation, severe pulmonary hypertension and ejection fraction of 25-30%. He was started on IV Cefazolin for expected 8 weeks of treatment for TV endocarditis. Psychiatry recommended initiating Gabapentin and Sertraline for anxiety. Cardiothoracic surgery declined offering surgical repair because of ongoing drug use.
Psychiatry was re-consulted to help co-manage the patient’s anxiety and substance misuse, recommending in-hospital buprenorphine induction given his daily heroin use and desire for positive change. Following initiation of buprenorphine, the patient reported minimal cravings or withdrawal symptoms and had no additional substance use. He discharged to his parents’ home after successfully completing inpatient IV antibiotics.
Post discharge, he followed with an outpatient psychiatrist for continued management of opioid dependence with buprenorphine and attended regular opioid recovery groups. On re-evaluation by CT surgery, the patient was offered and received TV replacement in light of his continued sobriety.
Discussion: Tricuspid valve bacterial endocarditis in individuals who inject drugs is well documented. Given the risk of valvular infection post valve repair or replacement with continued injection drug use, this patient population is frequently not offered surgical interventions despite medical indication.
This case illustrates (1) the value of in-hospital buprenorphine induction to help individuals with opioid-dependency access medically indicated surgical treatment for endocarditis, and (2) the critical role of in-hospital interdisciplinary management of medical, psychiatric and substance use problems for improved patient outcomes. Initiating buprenorphine in the hospital with minimal delay can be potentially lifesaving for those who need it. Yet despite evidence supporting opiate-replacement therapy as an effective treatment for opioid dependency, buprenorphine induction and linkage to maintenance is rarely offered in the hospital setting. Possible barriers include lack of physician training and experience with buprenorphine, provider biases against drug users, and insufficient resources for discharge planning.
Conclusions: In-hospital buprenorphine is currently underutilized. To increase the availability of this potentially life-saving therapy, institutions should consider expanding provider training as well as establishing hospital policies and protocols to facilitate buprenorphine initiation and maintenance.