Background: On January 1st, 2017, the Joint Commission antibiotic stewardship accreditation standard came into effect, requiring hospital wide antibiotic stewardship programs. In West Virginia, per the CDC, in 2014, less than 28% had a stewardship program that met all 7 of the CDC core elements. In a May 2017 article of Clinical Infectious Diseases, authors concluded that one of the most significant barriers for small hospitals is a lack of dedicated ID-trained staff to support antibiotic stewardship, and surveys of smaller hospitals showed that access to ID physicians are around 50%. There have been a limited number of studies published around antibiotic stewardship in acute care rural hospitals.
Purpose: Purpose is to highlight a resident led, internal medicine hospitalist attending supervised, development of an antimicrobial stewardship program at a rural community hospital in West Virginia.
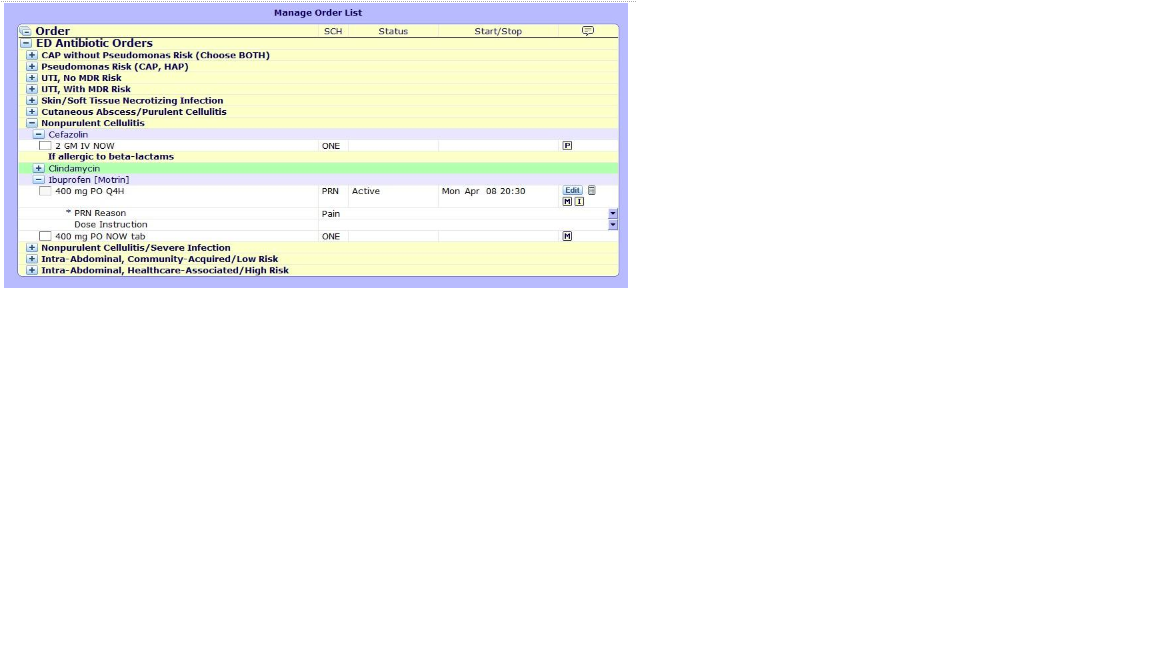
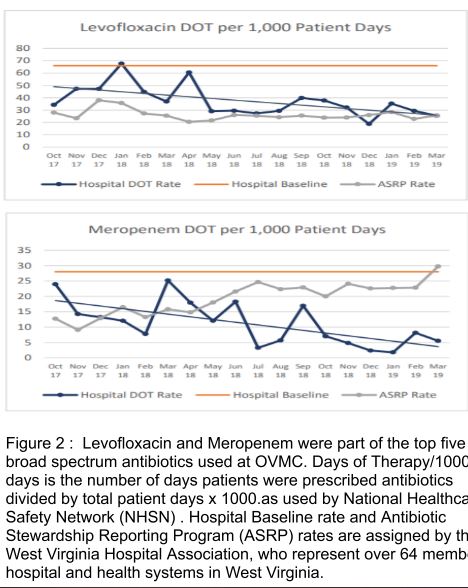
Description: Ohio Valley Medical Center is a 200-bed underserved community hospital in Wheeling, WV. It is affiliated with West Virginia School of Osteopathic Medicine with an internal medicine/emergency medicine residency. The hospital recently has been going through financial distress limiting available resources and had limited infectious disease support. Stewardship team was resident led with oversight from internal medicine attendings with multi-disciplinary teams. Antimicrobial stewardship efforts were focused on low cost, high yield measures that resulted in the goals of (1) meeting compliance of Joint Commission Standard seven core guidelines (2) standardization of infectious disease management processes (3) improving education. Antibiotic order sets were created for urinary tract infections, pneumonia, intra-abdominal infections, surgical site prophylaxis and skin/soft tissue infections. Quality improvement projects by internal and emergency medicine residents include but not limited to creation of an antibiotic time out note to encourage re-evaluation of antibiotics usage, beta lactam allergy assessment, and review of appropriate ordering of urinalysis in asymptomatic bacteriuria and blood cultures in the emergency room. Although limited in our ability to gather robust data, we have seen a decrease in antibiotic usage with meropenem (baseline of 28 to 9 ) and ertapenem (baseline of 16 to 7) in Days of Therapy and a 95% clinical pharmacist interventions acceptance rate.
Conclusions: Our goal was to highlight the journey of a resident led, hospitalist faculty supervised antibiotic stewardship program in a resource limited environment.