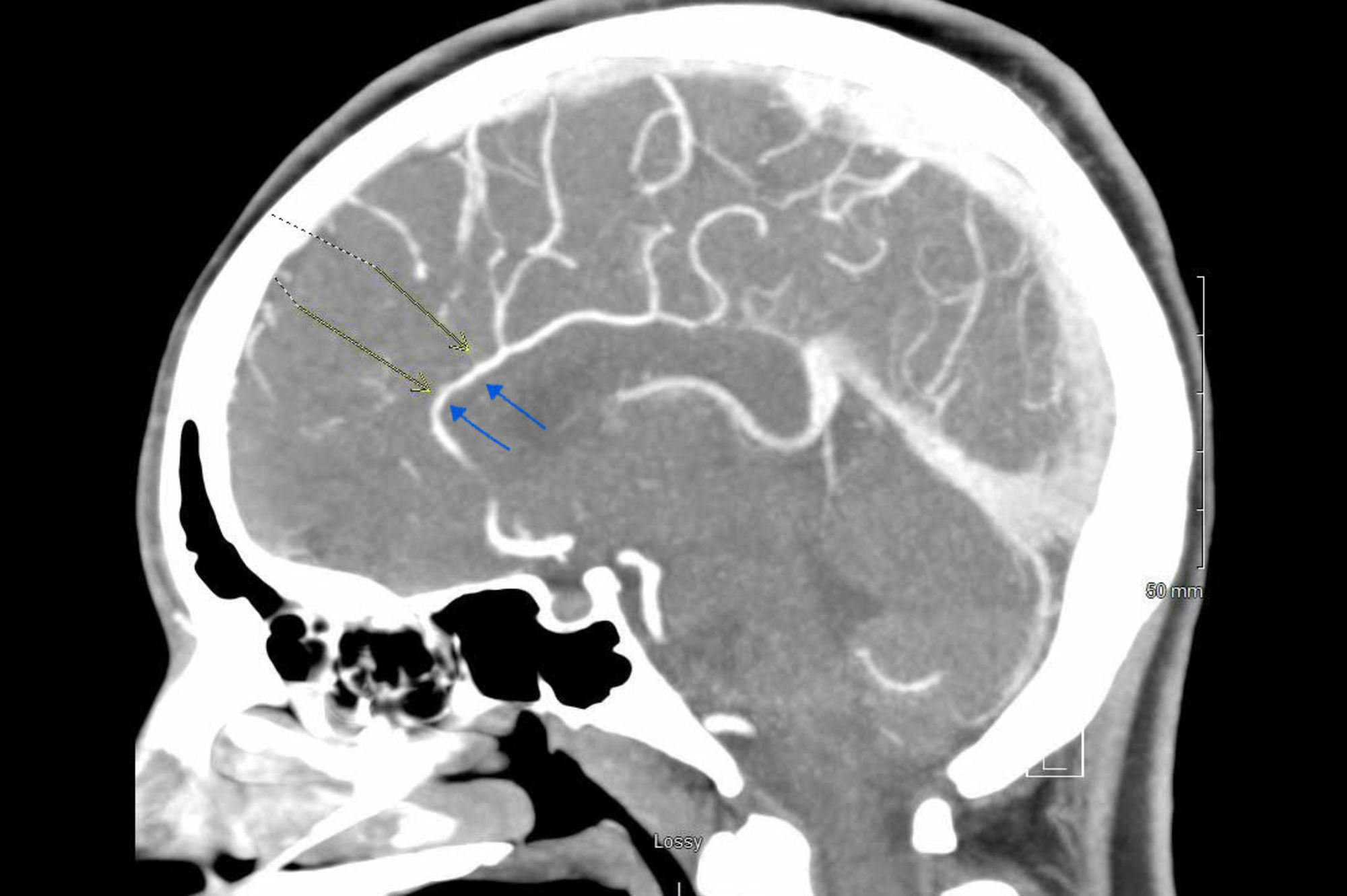
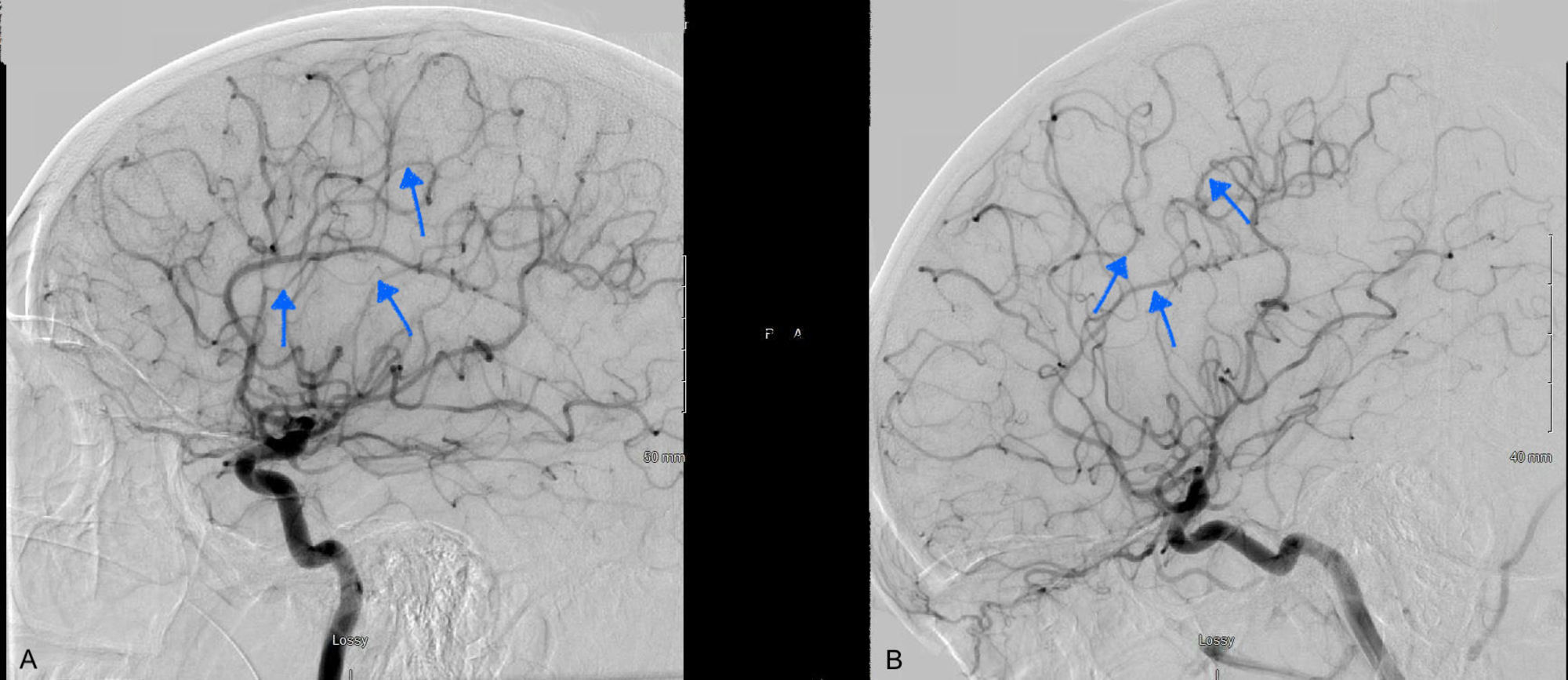
Case Presentation: 23-year-old female was admitted with thunderclap headaches of 2 days. She had a history of quadriplegia and autonomic dysreflexia from a remote cervical spinal cord injury and has been on midodrine for 2 years. She also reported blockage of the urinary catheter and experienced recurrent headaches when she attempted to flush the catheter. There was no change in the neurological examination from her baseline. CT head revealed subarachnoid hemorrhage (SAH). CTA head was remarkable for multifocal narrowing of the anterior cerebral artery, bilateral middle cerebral arteries (MCA), right posterior cerebral artery.Lab workup consisting of CBC, CMP, ESR, comprehensive drug screening, ANA, ANCA panel, and angiotensin-converting enzyme, were within normal limits.The diagnostic cerebral angiogram was remarkable for stenosis of the bilateral posterior cerebral arteries, right anterior cerebral artery, and right middle cerebral artery. During her hospital stay, her headaches recurred, which were associated with episodes of flushing, sweating, and elevated blood pressure. These events were precipitated by unclogging or flushing her foley catheter. Midodrine was discontinued and her headaches improved significantly at the time of discharge. Three months after discharge from the hospital, she underwent repeat diagnostic cerebral angiogram, which was unremarkable thereby confirming Reversible Cerebral Vasoconstriction Syndrome (RCVS). The patient denied a recurrence of symptoms during the subsequent follow-up visit.
Discussion: Autonomic dysreflexia is a neurological condition seen in patients with complete or partial spinal cord injury at or below the level of T6 manifested by an episodic rise in blood pressure, variability in heart rate, anxiety, headache, flushing, and sweating[3-6]. Severe cases can also have cerebral and spinal SAH and flash pulmonary edema[7]. These are often precipitated by a noxious stimulus to the bladder, bowel, and skin surface below the level of injury. This leads to a massive release of sympathetic mediated noradrenaline and dopamine from the splanchnic vascular bed, which causes severe vasoconstriction, resulting in a sudden rise in blood pressure, skin pallor, and piloerection below the level of the lesion[8]. Our patient experienced similar episodes of flushing, diaphoresis, high blood pressure, and severe headache following bladder distention and flushing of the foley catheter.About 74% of patients with spinal cord injury have orthostatic hypotension and 59% of patients were found to be symptomatic[9]. The index patient had orthostatic hypotension in the past and was started on midodrine after she failed the non-pharmacological interventions. Midodrine is an α-adrenergic agonist that causes peripheral vasoconstriction[9]. Our patient experienced an episodic massive sympathetic response due to noxious stimuli resulting from the bladder distention and manipulation of the foley catheter. This, along with the use of midodrine, caused vasoconstriction of major cerebral vessels and endothelial damage resulting in RCVS and SAH. The patient’s symptoms resolved after the discontinuation of midodrine.
Conclusions: RCVS should be considered as one of the differentials in patients presenting with a thunderclap headache in the context of the usage of vasoactive agents, serotonergic drugs, or sympathomimetic agents. Caution needs to be exercised while using vasospastic agents, such as midodrine, in patients with autonomic dysreflexia.