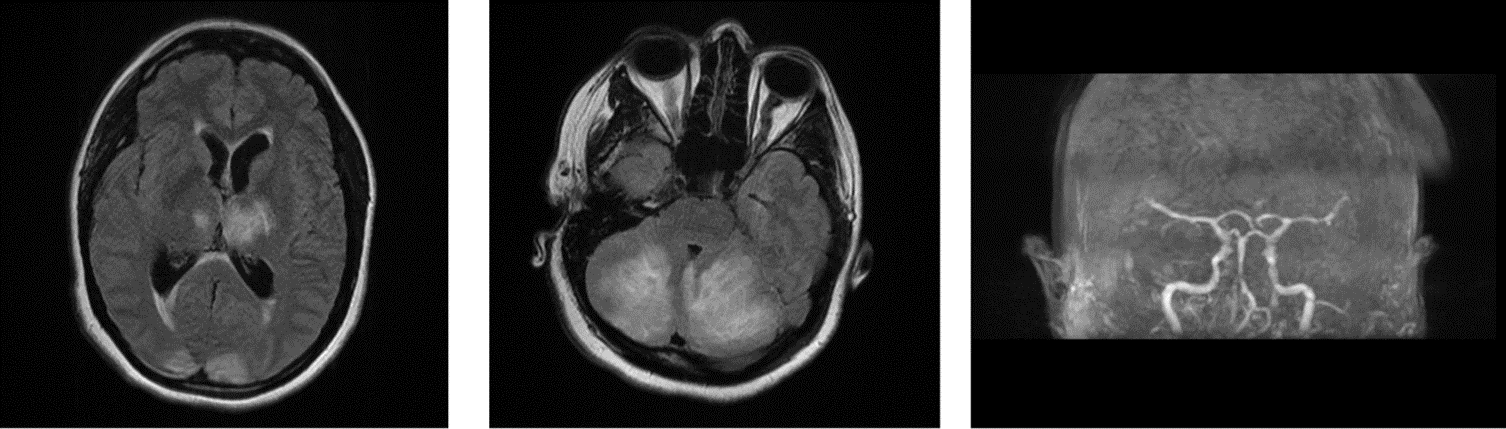
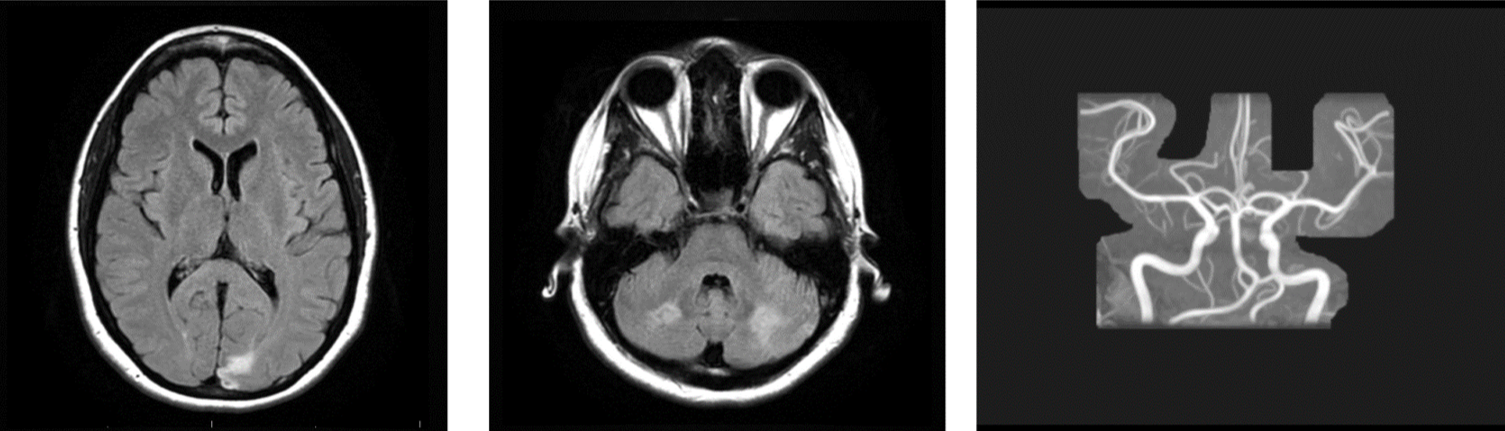
Case Presentation: We present a case of a 41-year-old female with a history of hypertension and anxiety who presented with severe headache, palpitations, and nausea for 1 day. Suspecting it to be a case of migraine, she was given diphenhydramine, ketorolac, and metoclopramide. Immediately after receiving metoclopramide she experienced a tonic-clonic seizure and became tachycardic. She received Ativan and was intubated for airway protection. CTH obtained was normal. CTA chest obtained for persistent tachycardia revealed large right adrenal mass raising suspicion for pheochromocytoma. a and b adrenergic blockade was initiated. Plasma metanephrines obtained returned significantly elevated. The patient’s condition stabilized over the next few days, however, post-extubation she was found to have dysarthria and visual field defects. MRI brain showed cerebellar swelling and multiple subacute infarcts in cerebellar hemispheres, bilateral thalami and occipital and parietal lobes with associated T2 FLAIR. MRA head and neck was concerning for basilar artery narrowing which raised suspicion for cerebral vasculitis. Stroke neurology suspected the subacute strokes to be hypertensive in nature in the setting of catecholamine crisis rather than secondary to basilar artery narrowing. Since the patient did not have any neurological symptoms prior to her presentation, further workup was deferred and the decision was made to watch patient clinically. Interval CT head 48 hours later showed stable cerebellar swelling without new infarcts. She underwent uncomplicated partial right adrenalectomy after appropriate BP and HR control. Histopathology was consistent with pheochromocytoma. 2 months after surgery repeat MRI brain showed chronic infarcts in left occipital and bilateral cerebellar hemispheres. Comparing MRI to previous scans there had been an improvement in the FLAIR changes. MRA head and neck was negative for basilar artery narrowing. 8 months after her initial presentation she continues to experience mild dysarthria.
Discussion: Reversible cerebral vasoconstriction syndrome (RCVS) is a group of syndromes characterized by reversible segmental constriction of cerebral arteries. RCVS is suspected to be an important cause of the paroxysmal neurological symptoms and neurological complications during acute catecholamine crises. Angiography shows a reversible multifocal narrowing in large and medium-sized cerebral arteries. High levels of circulating catecholamines are thought to be the causes of this reversible vasoconstriction. Complications of RCVS include subarachnoid and intracerebral hemorrhage, seizures, transient ischemic attacks, and cerebral infarction.Even though our patient did not undergo angiography, the MRI brain showed narrowing of the Basilar artery raising suspicion for vasoconstriction. It is important to recognize RCVS as angiographic finding closely resemble that of cerebral vasculitis. This distinction is especially important in the case of pheochromocytoma as cerebral vasculitis is treated with steroids which can also trigger an acute catecholamine crisis.
Conclusions: RCVS is an important but mostly reversible mechanism that can complicate acute catecholamine crisis. It is important to recognize and differentiate this syndrome from cerebral vasculitis to avoid steroid exposure as retrospective studies have shown worse outcomes in patients with RCVS who received steroids.