Background:
Increased mortality has been observed for patients admitted on weekends to hospitals in several studies. The reasons for this “weekend effect” are unclear but may be related to reduced staffing levels, increased handoffs, or reduced availability of diagnostic or therapeutic services. The ability to easily and accurately assess mortality trends based on the day of week is of great interest. Risk‐adjustment methodologies, such as those developed by the University HealthSystem Consortium (UHC), may have an advantage over gross outcome measures, which may hide clinically meaningful trends because of confounding variables. The risk‐adjustment model used in the UHC clinical database generates regression models based on patient characteristics such as age and comorbidities that can calculate an expected mortality for each individual patient. As such, a mortality index based on the UHC model may be helpful in elucidating mortality trends like those described with the weekend effect. These risk‐adiusted models are readily available to many institutions as a result of the increasing focus on delivering quality health care.
Purpose:
Our objective was to describe the weekend mortality trends with available administrative data from a large teaching hospital, using the University HealthSystem Consortium (UHC) risk‐adjustment methodologies.
Description:
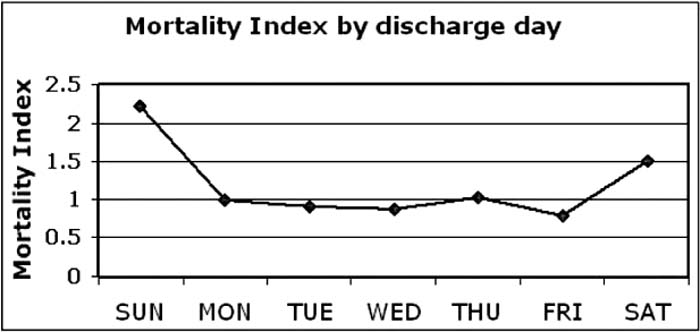
Administrative data sets for expected and observed inpatient mortality, organized both by day of admission and day of discharge, were collected for 14,388 discharges at the study institution from the fourth quarter 2007 to the third quarter 2008. Interventional cardiology patients and length of stay outliers were excluded. A mortality index was calculated by dividing the observed mortality by the expected mortality. Mortality indices were then calculated for each patient based on their day of discharge or day of admission. Mortality data prior to risk adjustment demonstrate fewer deaths on weekends and more deaths on weekdays, ranging from 68 total deaths on Sundays to 103 deaths on Wednesdays. A mortality index based on day of admission was close to 1 (range 0.95–1.08) on weekdays, but an index of 1.20 and 1.04 was observed on Saturdays and Sundays, respectively. When the data were grouped by discharge day, the mortality index calculated to 1.51 and 2.22 on Saturday and Sunday, respectively, while the weekday mortality ranged from 0.80 to 1.03.
Conclusions:
UHC‐derived administrative data suggest a higher mortality for patients discharged on weekends and suggest higher mortality for patients admitted on Saturday. This mortality difference is not evident when looking at raw mortality data alone. Administrative data sets with risk adjustment may be useful to hospitalists interested in monitoring quality and mortality trends in the hospital. Future investigation will focus on identifying why mortality indices are higher on weekends, including possible staffing shortages or a higher number of handoffs.
Author Disclosure:
R. Jervis, none; N. Kathuria, none; E. Rule, none; D. Chang, none; L. Mumm, none.