Background: In 2020, COVID-19 emerged as the third leading cause of mortality in the United States with high death rates in urban areas at the beginning of the pandemic. By December 2020, the COVID-19 mortality pattern changed with higher mortality in rural areas.1,2 Epidemiological studies showed that rural populations were at a higher risk of serious COVID-19-related illness with high rates of hospitalizations.3 In the United States, adults in rural compared with urban communities have higher rates of short-term mortality and readmission rates following hospitalization for COVID-19. However, differences in the long-term outcomes are unknown.We compared long-term mortality and readmission rates following COVID-19 hospitalization by rural-urban residential status.
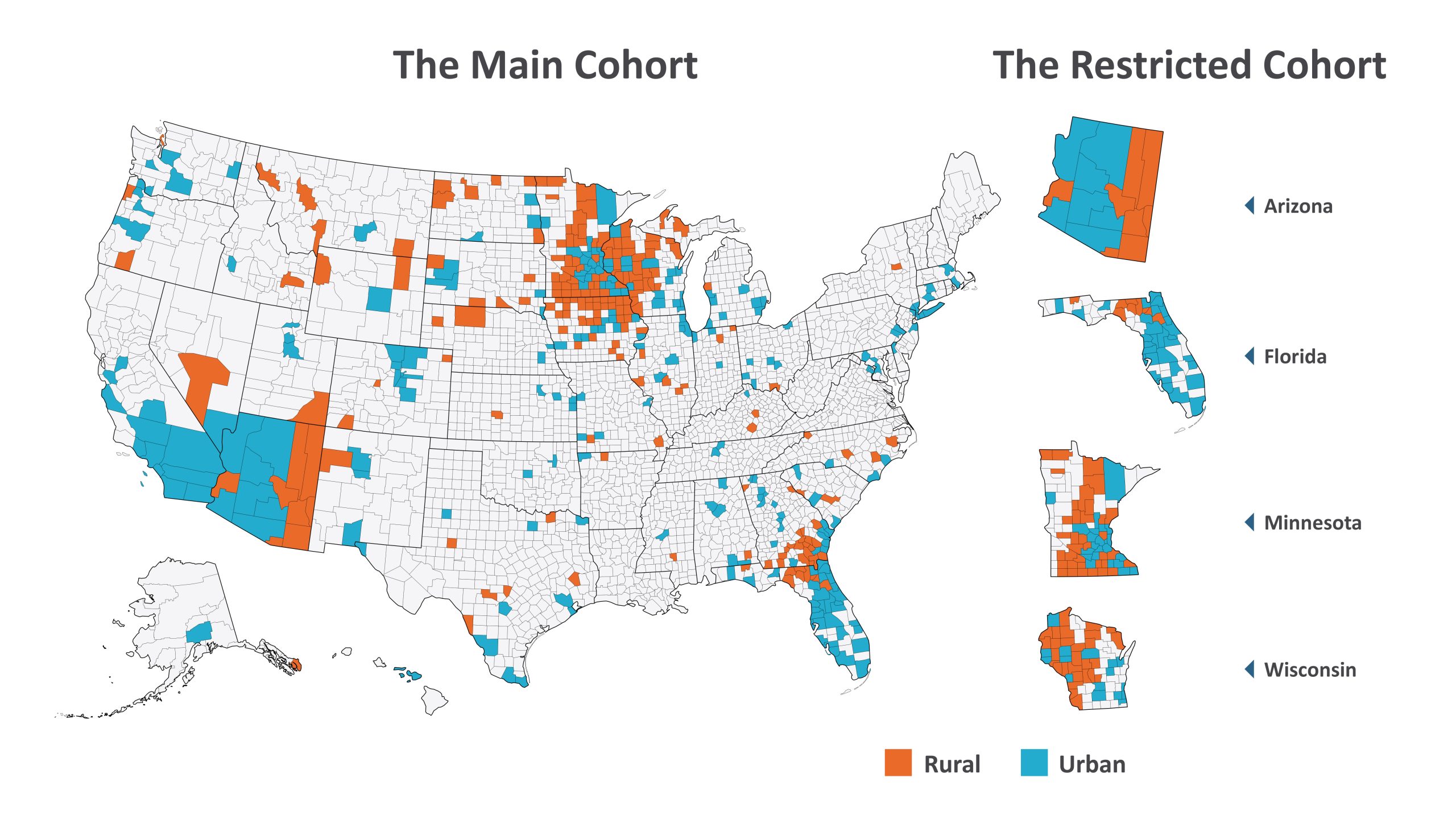
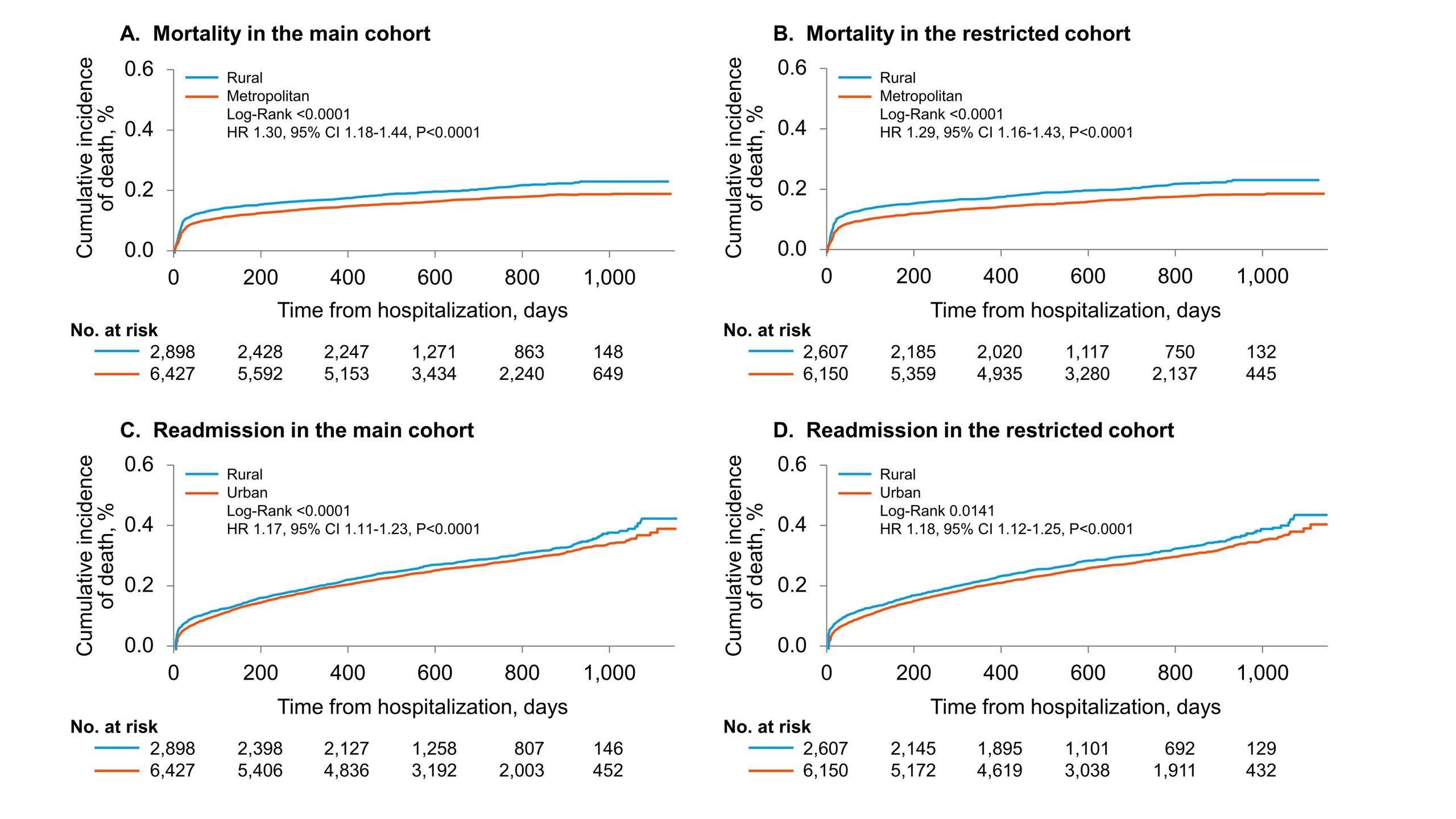
Methods: A retrospective cohort study of 9325 patients admitted with COVID-19 at 17 hospitals in 4 U.S. states between March 1, 2020, and July 22, 2022, with follow-up through May 23, 2023. For data analysis, we considered two separate cohorts: (1) the main cohort with all patients regardless of residency in the U.S. and (2) a restricted cohort with patients from the U.S. states with the study centers. Rurality was assigned by the patient’s county of residence and classified as rural (nonmetropolitan) or urban (metropolitan).Rural-urban differences in mortality and readmission were estimated using Kaplan-Meier estimates and multivariable Cox regression models in both the main and restricted cohorts. Subgroup analyses were conducted according to age, sex, race, marital status, pandemic year, and in-hospital medications.Rural-urban differences in mortality and readmission were estimated using Kaplan-Meier estimates and multivariable Cox regression models in both the main and restricted cohorts. Subgroup analyses were conducted according to age, sex, race, marital status, pandemic year, and in-hospital medications
Results: The main cohort consisted of 9,325 patients hospitalized with COVID-19: 31% of patients were from 187 rural counties in 31 states and 69% from 234 urban counties in 44 states. The mean age was 65 years (rural, 66 years; urban, 64 years). There were 3894 women (rural, 41%; urban, 42%); 8007 whites (rural, 87%; urban, 83%); 1738 deaths (rural, 21%; urban, 17%); and 2729 readmissions (rural, 30%; urban, 29%). Over a median follow-up of 602 days (interquartile range, 462-856 days), in the main cohort, rural residence was associated with a 30% higher all-cause mortality (adjusted hazard ratio [aHR] 1.30, 95% confidence interval [CI] 1.1-1.44), and 17% higher readmission rate (aHR 1.17; 95%CI 1.11-1.23). The results in the restricted cohort (n=8757 total; rural, 30%; urban, 70%) were robust with those of the main cohort with consistent findings across most subgroups.
Conclusions: Rurality was independently associated with higher long-term mortality and readmission rate following initial COVID-19 hospitalization and warrant further studies into the mechanisms to mitigate rural-urban disparities.