Background: Health professionals providing care to patients of limited English proficiency (LEP) are mandated by federal law to provide adequate language interpretation. Professional medical interpreters are associated with an improvement of health outcomes for patients with LEP due to decreased communication errors, improved patient comprehension, and improved overall patient satisfaction.1 However, professional medical interpreters are underutilized in clinical settings.2 This study aimed to identify the barriers to effective medical interpretation of languages by physician trainees at an academic medical center.
Methods: Internal medicine residents and fourth year medical students were surveyed to assess barriers to utilization of interpretation services in their clinical roles. The survey primarily served to identify if a perceived barrier to utilization existed, and secondarily to identify the types of barriers experienced. Respondents were then asked to identify the most significant barrier they have experienced and suggest possible solutions. The survey finally asked if respondents received formal training on patient communication using interpreters.
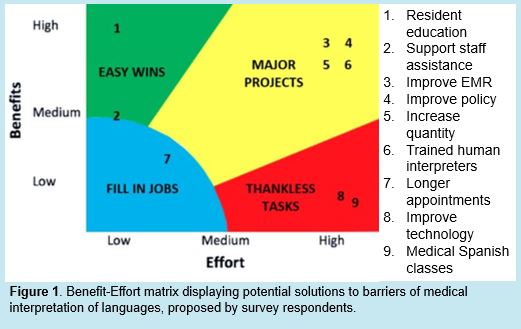
Results: 159 surveys were completed. In the inpatient setting, 93% of respondents experienced barriers to medical interpretation. Most commonly encountered barriers included access to interpretation services (72%), time constraints (76%), and overestimation of patient understanding (58%). 42% considered access to be the most significant barrier, while 43% considered time to be most significant. Only 21% of respondents indicated that they received formal training on communication using medical interpreters in medical school. Potential solutions proposed by respondents are depicted in a Benefit-Effort matrix (Figure 1).
Conclusions: In this single-center study, the vast majority of trainees identified barriers to effective communication with patients of LEP. In the inpatient setting, lack of time and physical access to interpretation services were most impactful. Ineffective communication may have a detrimental impact on patient safety, health care quality, and patient satisfaction. Potential solutions to improve the use of interpretation services have been posed. Given the reported lack of targeted training in this area, one solution with maximal benefit and minimal effort would include formalized resident education focused on effective and efficient communication with patients of LEP. Further studies implementing this and other solutions should be completed on a broader scale to evaluate their effects on health care quality and patient satisfaction.