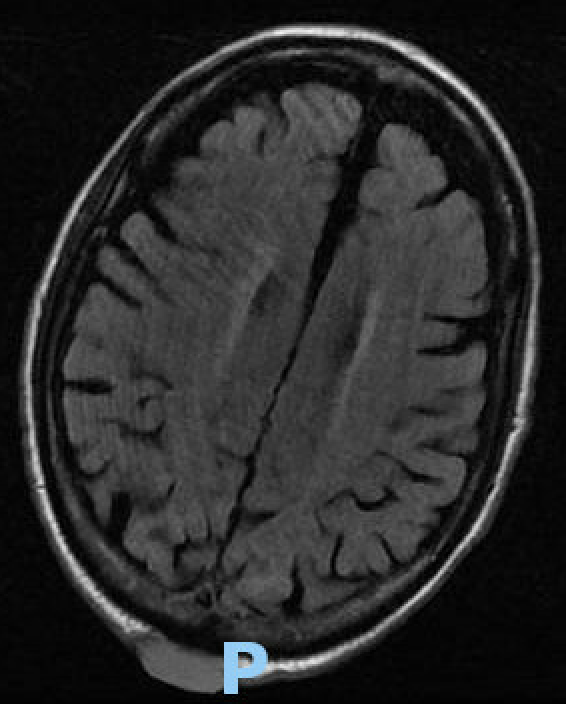
Case Presentation: A 75-year-old male with a history of left upper lobe neuroendocrine lung cancer in remission presented to the hospital with progressive diplopia and headaches for 4 weeks. Prior to admission, he had recently been diagnosed with squamous cell carcinoma (SCC) on the vertex scalp which appeared at the onset of diplopia. Histology showed moderately differentiated SCC, however no connection to epidermis. The PET/CT skull base to mid-thigh scan revealed a 2.9 x 1.1 cm intensely F-18 fluorodeoxyglucose (FDG)-avid cutaneous nodule at the occipital region, an ill-defined focus of intense activity in the inferior right lobe of the liver, and an enlarging and increasingly intense focus (3.4 x 1.6 cm) of uptake at the right hilum. His hospital course was notable for significant bilateral cranial nerve six palsies on examination. A brain MRI showed an abnormal marrow signal involving the clivus with soft tissue extension into the bilateral cavernous sinuses. Fine needle aspiration of the previously identified hepatic lesion was performed and immunohistochemistry revealed strongly positive P40 and negative TTF1 markers. Based on the pathology results, a diagnosis of metastatic lung squamous cell carcinoma was made. While aggressive treatment options, including radiation therapy, were discussed, the patient and family ultimately opted for hospice care, prioritizing comfort and quality of life.
Discussion: This case highlights a rare and clinically significant presentation of metastatic lung SCC. Prior to admission, a scalp lesion was diagnosed as SCC, raising a diagnostic dilemma: whether the lesion represented a primary cutaneous malignancy or metastatic disease. Imaging and biopsy confirmed widespread metastases involving the brain, liver, and lungs, with histopathologic findings favoring pulmonary origin. Notably, the scalp lesion was determined to be metastatic, as it lacked epidermal connection, and immunohistochemical staining (p40 positive, TTF-1 negative) further supported the lung as the primary site. While lung SCC frequently metastasizes to the liver, brain, and other distant sites, the initial presentation with a scalp lesion and cranial nerve VI palsy from clivus involvement is highly unusual. The patient’s diplopia was traced to the clival metastasis, highlighting a rare but significant complication of metastatic disease. This presentation underscores the potential for atypical metastatic patterns in lung SCC and the diagnostic complexity they pose. Multidisciplinary care was critical in navigating this patient’s complex clinical scenario and ensuring patient-centered goals and quality of life.
Conclusions: Recognizing atypical presentations of metastatic lung SCC, such as scalp lesions and cranial neuropathies, requires a high index of suspicion, especially in patients with a history of lung cancer. This case underscores the importance of histopathology and immunohistochemistry in determining the origin of ambiguous lesions and the need for a multidisciplinary approach to guide management.