Scheduling Follow-Up Appointments Prior to Discharge: Analysis of Project Impact Pilot Data
Clare Ronan, BA, Tufts University School of Medicine, Portland, ME; David Cooperberg, MD, St. Christopher's Hospital for Children, Philadelphia, PA; Sandra Gage, MD, PhD, Medical College of Wisconsin, Milwaukee, WI; Snezana Nena Osorio, MD, MS, Weill Cornell Medicine, New York, NY and Leah Mallory, MD*, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME
Abstract Number: 175
Background:
Project IMPACT (Improving Pediatric Patient-Centered Care Transitions) is a multi-center quality improvement collaborative aiming to improve hospital to home transitions. As part of this project, providers attempt to schedule follow-up visits prior to discharge and conduct post-discharge phone calls.
Objective:
1.Determine relationship between scheduling post-discharge follow-up visits and 30-day reutilization rates
2. Characterize patients not scheduled for follow-up visits and unable to be reached via post-discharge phone call: at risk for lost to follow up (LTFU)
Methods:
Demographic, visit and follow up data were collected via electronic health record review and post-discharge phone call transcripts from 4 sites between January 2014 and June 2015. Χ2 analysis compared patients scheduled for a follow-up visit versus not, and patients LTFU versus not.
Results:
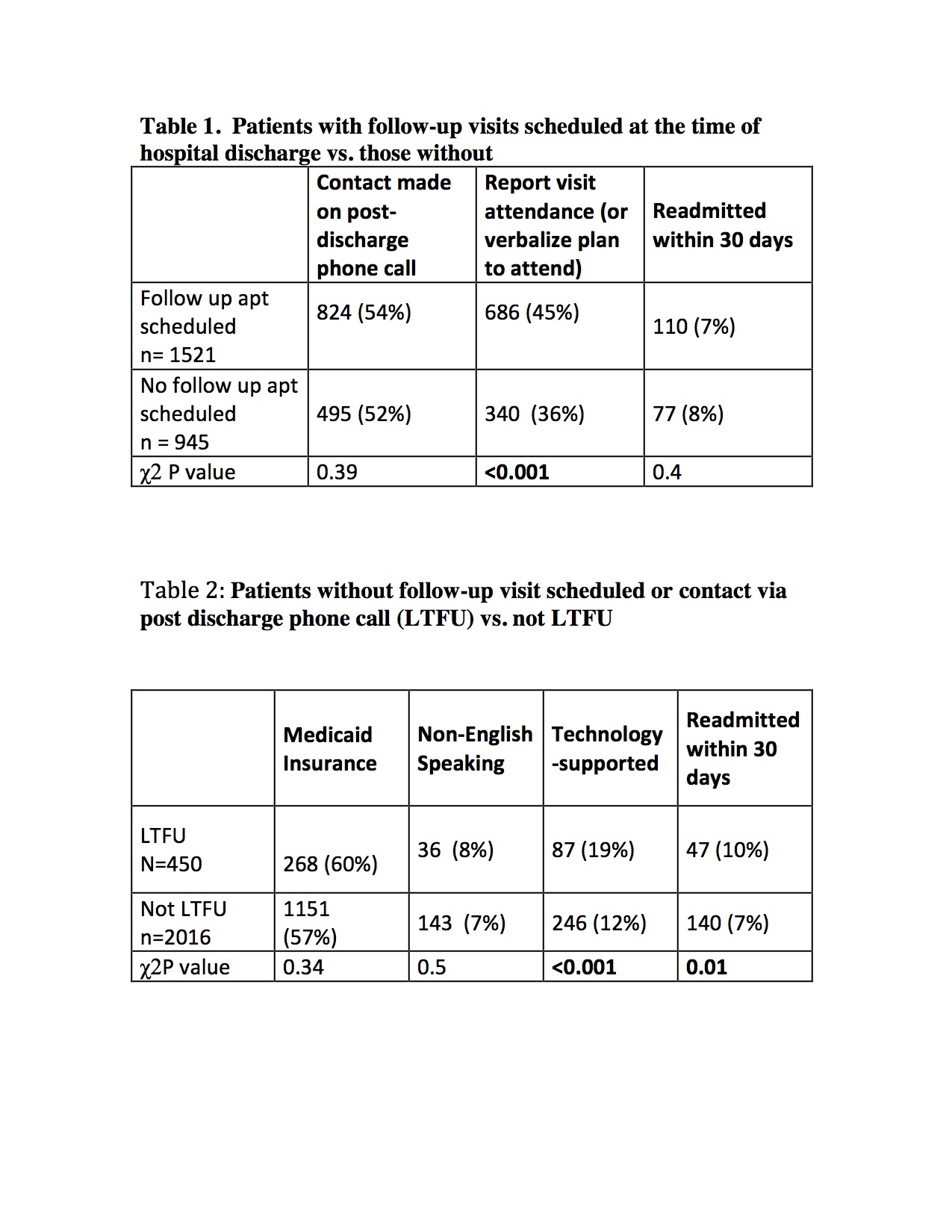
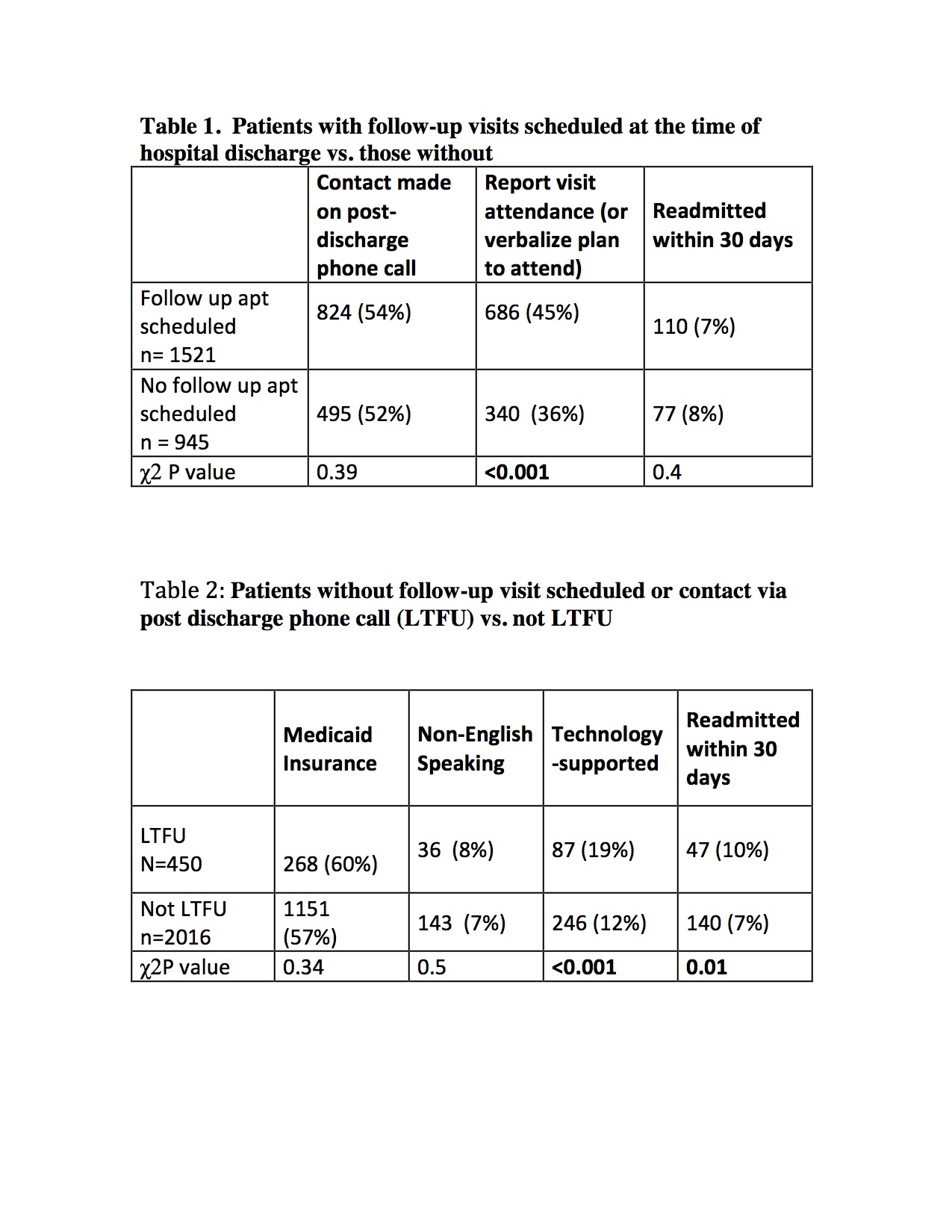
We reviewed 2466 cases, 824 had follow-up visits scheduled. Readmission rates were not associated with scheduled follow up. [Table1] Patients at risk for LFTU (18%) were more likely to be technology–supported and readmitted within 30 days. [Table 2]
Conclusions:
Scheduling follow-up visits was not associated with a universal decrease in readmissions. A fifth of all discharged patients had no follow-up visit scheduled and could not be reached at the time of post-discharge phone call. These patients were more likely to be
technology-supported and readmitted indicating the possible benefit of identifying these patients prospectively in order to bolster transition supports for this group.
To cite this abstract:
Ronan C, Cooperberg D, Gage S, Osorio SN, Mallory L.
Scheduling Follow-Up Appointments Prior to Discharge: Analysis of Project Impact Pilot Data.
Abstract published at Hospital Medicine 2016, March 6-9, San Diego, Calif..
Abstract 175
Journal of Hospital Medicine, Volume 11, Suppl 1.
https://shmabstracts.org/abstract/scheduling-follow-up-appointments-prior-to-discharge-analysis-of-project-impact-pilot-data/.
February 10th 2026.