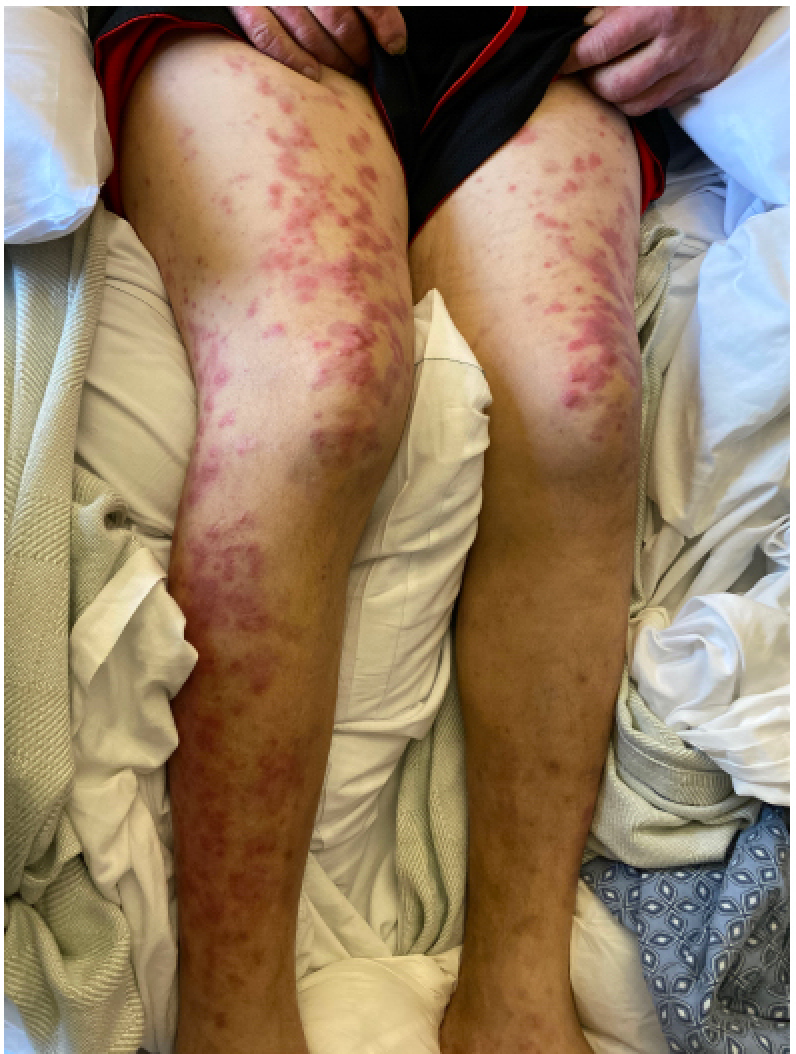
Case Presentation: A 45-year-old male with a past medical history of Myelodysplastic Syndrome, Atrial Fibrillation, and Type 2 Diabetes presented for evaluation of worsening diffuse, erythematous, and painful rash all over his body. The rash initially began 2 months ago and was biopsied at an outside hospital. The biopsy was read as a “dermal hypersensitivity reaction” and suspected to be secondary to Stevens-Johnson Syndrome secondary to his prescription allopurinol. The patient was discharged with a 6 week course of prednisone with initial improvement however the recurrence of his rash along with additional fevers and shortness of breath prompted the patient to present for evaluation.In the emergency department, the patient was noted to be tachycardic, with all other vital signs normal. Labs were significant for a hemoglobin of 6.7, platelet count of 71 and lactic acid of 4.1. Given his acute presentation of a rash in the setting of his myelodysplastic syndrome, both Dermatology and Oncology were consulted and he was started on methylprednisolone 125 mg BID. Given his worsening progression, both bone marrow and skin biopsy were performed on day 3 of this hospitalization. The bone marrow biopsy was reviewed as ”Acute Myeloid Leukemia with 40% blasts with erythroid and myeloid dysmaturation” and his skin punch biopsy was read as “lichenified skin with no fungal elements”. His rash was initially believed to be a drug reaction to his prophylactic antibiotics and his trimethoprim /sulfamethoxazole was held.Despite this intervention, his rash continued to spread and the patient continued to have persistent tachycardia, leukocytosis, and fevers. Due to high clinical suspicion for Sweet Syndrome, a repeat punch biopsy was performed on Day 8 of hospitalization which revealed “Neutrophilic Dermatosis consistent with Sweet’s Syndrome”. Given the patient’s newly diagnosed AML he was started on inpatient chemotherapy with daunorubicin and cytarabine on day 14. The patient’s rash was noted to subsequently improve after cycle 1 of his chemotherapy and several days of the steroids.
Discussion: Sweet Syndrome, also known more formally as “Acute febrile Neutrophilic Dermatosis” is characterized by the sudden onset of painful, erythematous papules, plaques, and nodules on the skin with accompanying fever and leukocytosis. It is associated with various conditions including infection, inflammatory bowel disease, pregnancy, malignancy, and drug reaction. More commonly, the malignancy-associated Sweet syndrome is classically associated with acute myeloid leukemia. A diagnosis is officially made based off both clinical and lab findings. Biopsies classically show “dense neutrophilic infiltrate in dermis without vasculitis”. First line treatment includes systemic steroids, with colchicine or dapsone as second line agents.
Conclusions: Sweet Syndrome is a rather uncommon diagnosis not experienced directly by many physicians. Many other exanthems such as infections, drug eruptions, pyoderma gangrenosum, and bullous pemphigoid can manifest with similar findings. Thus, the diagnosis can easily be misdiagnosed as was the case in this presentation. The purpose of this case is to highlight an uncommon skin exanthem that can be easily overlooked by many physicians and took several attempts to identify with biopsy. However prompt recognition of the disease along with timely treatment of the underlying malignancy can result in improvement of this rare syndrome.