Background: Palliative care (PC) has been shown to improve the quality of life for patients facing life-threatening illness and their families. PC screening tools have been successfully used in identifying cancer patients in need of PC services and increase hospice utilization. However, a PC screening tool specific to hospitalized septic patients is lacking, despite sepsis accounting for more than 50% of all in-hospital mortality. Based on our hospital’s internal systematic reviews of all inpatient deaths and sepsis cases, we found that earlier involvement of PC service may have improved care for 12%-15% of patients with sepsis.
Purpose: The purpose of this project was to develop a screening tool to guide palliative care consultation in hospitalized septic patients.
Description: The daily operation of our hospital “Stop Sepsis Program” incorporates a multi-disciplinary approach, involving clinicians, nursing staff, and specialized sepsis nurse practitioners (NPs). Possible sepsis is identified by a Best Practice Alert (BPA) in our electronic medical record. A BPA is triggered when a patient meets a combination of criteria for systemic inflammatory response syndrome and suspected infection as identified by the patient’s staff nurse. As a result, all septic patients trigger at least 1 BPA. Dedicated Sepsis NPs address all BPAs from 7:00AM to 7:00PM.
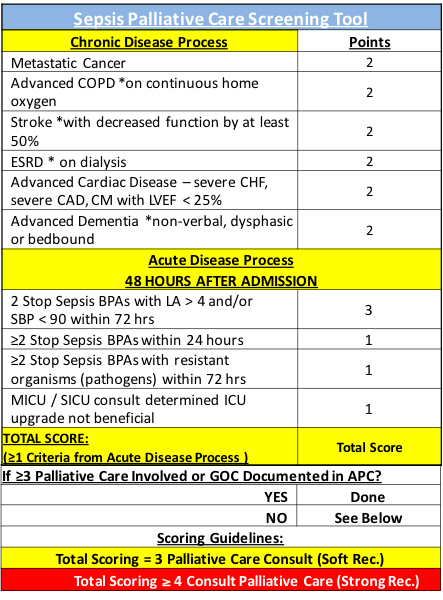
We adapted validated PC tools to our population of septic patients to create the Sepsis Palliative Care (SPC) tool. The tool was vetted by the Palliative Care and the Sepsis Teams, and piloted for 1 week prior to instituting it throughout the hospital. We hypothesized that a PSC score ≥ 3 would be associated with a high-risk of poor outcomes, including mortality.
Results: Both chronic diseases and the acute septic condition are assessed by the SPC tool. It utilized a point system where each criterion is assigned 1-3 points. For those cases where SPC scores were ≥ 3 and neither palliative care involvement nor documentation of advanced care planning was identified, the Sepsis NPs made a recommendation to the primary team to consult PC. A stronger recommendation was made for those with SPC score ≥ 4. (See Table)
During the 3-month intervention period, the Sepsis Team was activated on 1408 occasions, of which 69 had SPC scores ≥ 3, from 50 unique patients. The inpatient mortality rate of this group was 28%, and discharge to hospice was 40%. The total mortality until 30-day post-discharge was 46%, which is markedly greater than our hospital’s baseline sepsis mortality of 16%. Of those discharged to destinations other than hospice, the 30-day readmission rate was 35%. The mortality rate for readmissions was 43%. The overall average length of stay (LOS) was 34 days.
Of patients identified using the tool, 60% (n=30) did not have PC involvement at the time of screening. Seven out of 30 (23%) subsequently had PC consults. Compared to those without PC consults, those with consults were less likely to die while being full code (0/11 vs. 3/5), lower 30-day readmission rate (10% vs. 22%), and lower LOS (30.0 days vs 42.4 days).
Conclusions: The Sepsis Palliative Care screening tool identified patients with high rates of mortality, 30-day readmissions, and mortality on readmission. The SPC process prompted PC consultation for 23% of patients found to be at high risk by the SPC tool. PC involvement was associated with lower rate of death with full code, lower readmission rate, and a shorter average length of stay. These results suggest that SPC tool has the potential to aid efforts to improve care for patients with sepsis.