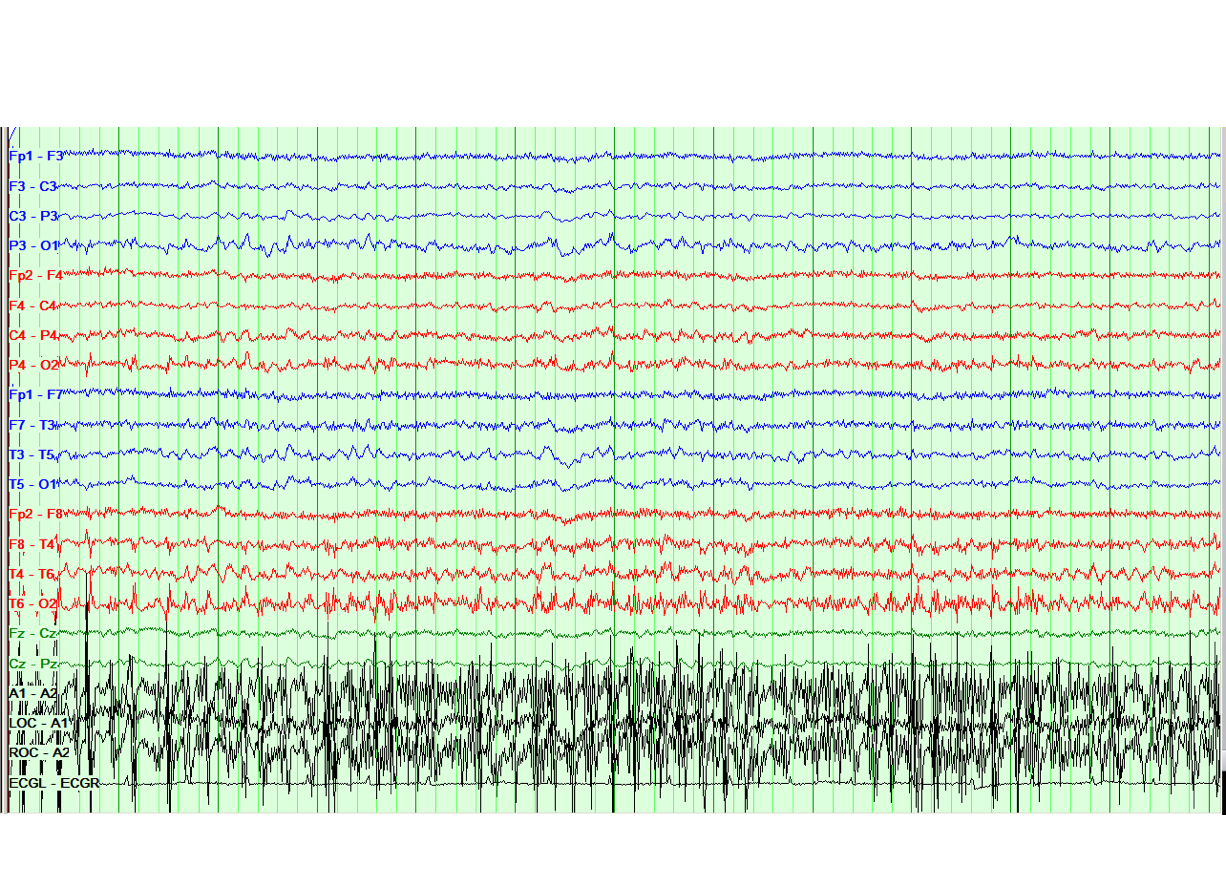
Case Presentation: An 82 year-old woman with history of stage five chronic kidney disease (CKD) presented with new onset of altered mental status, upper extremity tremors and slurred speech. Four days prior to presentation patient was diagnosed with urinary tract infection due to multidrug-resistant Pseudomonas aeruginosa, and was started on cefepime. On the day of presentation, she developed expressive aphasia, bilateral upper extremity tremors, and worsening general coordination. On admission, physical exam demonstrated prominent bilateral resting hand tremor, drowsiness, and poverty of speech. Lab work showed no change from her baseline blood urea nitrogen (BUN) and serum creatinine (Cr) levels. Serum electrolytes and thyroid stimulating hormone level were normal. Brain MRI did not demonstrate any acute intracranial abnormality. Given the fact that patient’s mental status was previously normal despite similar BUN and Cr levels, uremia was not considered a possible cause of her symptoms, and electroencephalogram (EEG) was obtained to evaluate for evidence of seizures. Phenytoin was also empirically started. EEG demonstrated stimulus-induced rhythmic periodic or ictal discharges (SIRPIDS), the characteristic finding of cefepime induced encephalopathy. Cefepime and phenytoin were therefore discontinued. Over the next 48 hours, the patient’s mental status returned to baseline and repeat EEG shows resolution of SIRPIDS.
Discussion: Hospitalists commonly encounter altered mental status. This case highlights the importance of avoiding anchoring bias by looking for alternative causes of altered mentation in the setting of uremia. Further, it teaches us to avoid injudicious use of antiepileptics. Sometimes, less is more and overtreatment can be detrimental to patient care. Cefepime induced encephalopathy, with SIRPIDS on EEG, is a rare but reported cause of altered sensorium with seizure activity, particularly so in patients with CKD as impaired renal function is implicated in cefepime associated encephalopathy due to failure in clearance of the medication. Management consists of discontinuation of the offending agent and supportive care.
Conclusions: Often in hospital medicine, a tentative working diagnosis is made early in the patient’s hospital course. This case emphasizes the fact that while a diagnosis may seem obvious, our first impressions are not always correct. It is also important to be mindful of the uncommon side effects of medications commonly prescribed in the hospital and to avoid anchoring bias with the final diagnosis, as it can cause unnecessary harmful interventions and sometimes, delayed treatment.