Background: Healthcare institutions have chronic bed shortages and a medically and socially complex patient population that makes optimal management of post-discharge care especially important. Effective and timely follow up post-hospitalization can improve clinical outcomes by delivering transitional care when patients are the most vulnerable. We developed a multimodal design that delivers education to patients and family members about their acute and chronic medical conditions, allows early identification of adverse events, and promotes medical adherence and a smooth transition to primary care providers.
Purpose: Our aims were to assess the PDC’s effectiveness of our transitional care interventions in our Post-Discharge Clinic (PDC) to decrease the 30-day rate of readmissions and Emergency Department return visits.
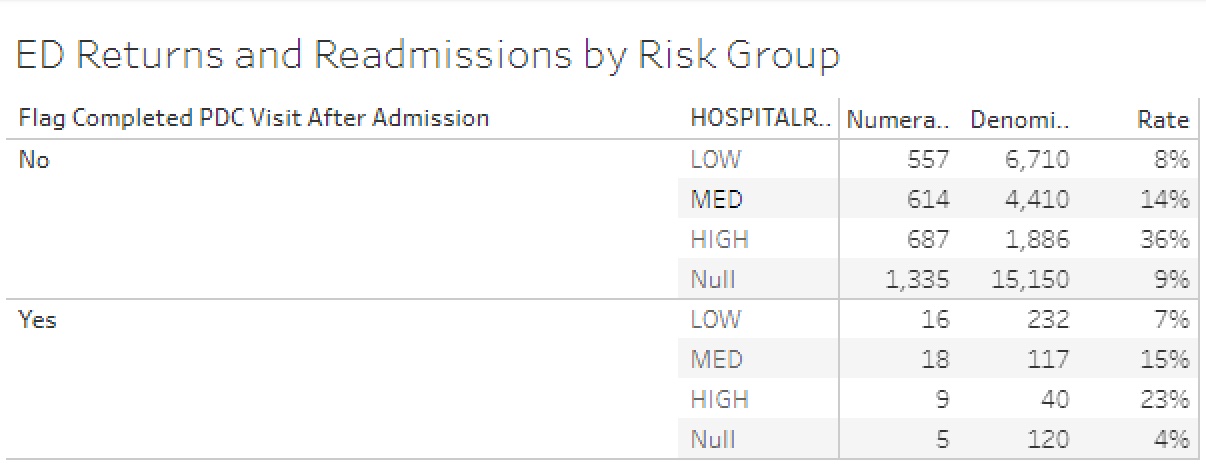
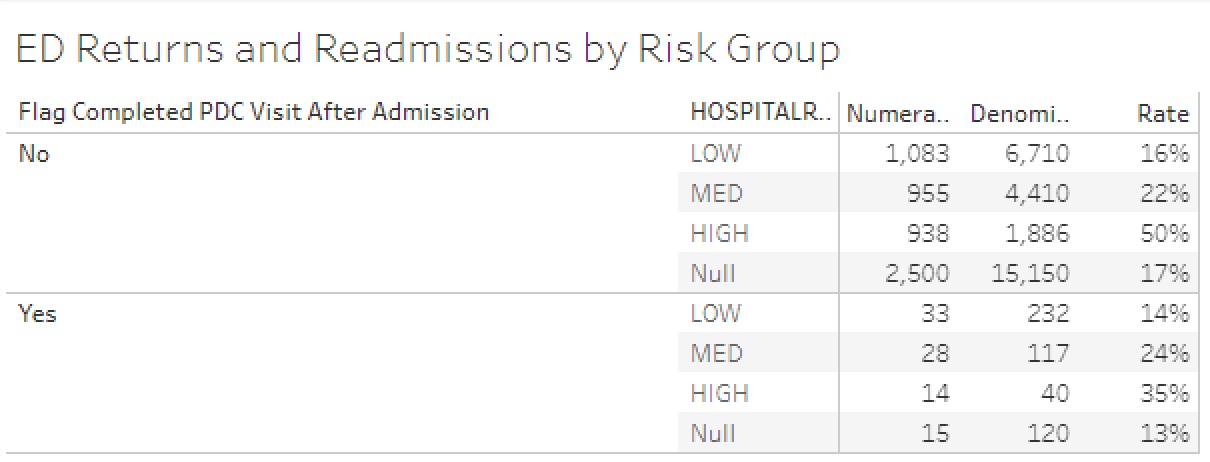
Description: The PDC created a multimodal care pathway to facilitate smooth transitions from inpatient to outpatient care. Three workflows were developed.1. Patient Identification: Patients are identified based on criteria that meets the needs of patients and providers, decreases length of stay and decreases the likelihood of readmission. Patients are identified by providers and that is communicated to the Patient Navigation Coordinators. 2. Scheduling: A novel self-scheduling system allowed Patient Navigation Coordinators (PNCs) to schedule patients directly in the PDC providers’ schedule. A shared folder in EPIC was created in which inpatient providers could enter the patient information for the PNCs to schedule.3. Clinic Flow: We mapped out a lean workflow. PDC visits were offered both in-person and virtually via MyChart and Doximity. The PDC partnered with finance to determine an out-of-network workflow. The PDC partnered with the Population Health team for 48-hour RN post-discharge phone visits. The PDC was able to participate in the Transitional Care Management (TCM) Program through both the timeliness of the visit as well as those TCM calls.Patients’ readmission and ED return rates were stratified by the Risk of Readmission Score and were compared for patients attending the PDC and patients not attending the PDC; data was surveilled by the Data Analytics Department. Our outcomes demonstrated:• PDC patients – readmission rate for high risk of readmission category within 30-days post-hospitalization: 23%• No PDC visit- readmission rate for high risk of readmission category within 30-days post-hospitalization: 36%• PDC patients- ED return rate for high risk of readmission category within 30-days post-hospitalization: 35%• No PDC visit- ED return rate for high risk of readmission category within 30-days post-hospitalization: 50%
Conclusions: We were able to identify and intervene on adverse events and measured the outcomes on 30-days readmission and ED return rates by risk groups. Patients seen at the PDC have 33% less readmission and ED return rates in the high-risk category compared to patients not seen at the PDC. The PDC shows improved access to post-discharge care and reductions in readmissions and emergency department visits.