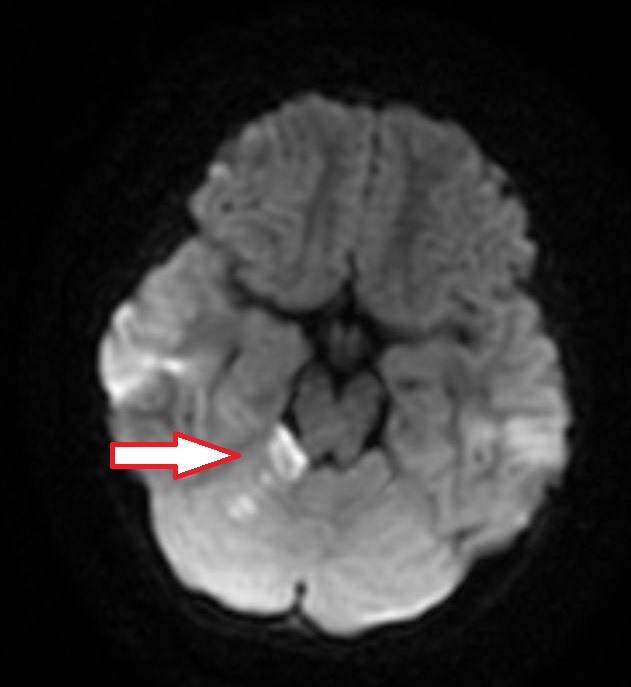
Case Presentation: A six-year-old female presented with ataxia and vomiting. She was running and fell, striking her forehead on the ground. There was no loss of consciousness. She got up and continued to play. About an hour later, she had difficulty feeding herself, trouble walking and started vomiting. The patient had no history of fevers, headaches, recent illnesses, ingestions, easy bruising or bleeding. She had a history of patent foramen ovale and a small ventricular septal defect that resolved. On exam, she was somnolent but arousable. She would not speak but could follow commands. She leaned toward the right when sitting up and fell when trying to walk. She had right dysmetria on cerebellar testing. Her head CT was normal. MRI and MRA revealed an acute right superior cerebellar infarct.
Discussion: Acute ataxia is uncommon presentation in children. When it does present, it is often due to a post-infectious cerebellar ataxia or an intoxication. Stroke is even less common, especially in healthy and medically uncomplicated children. Data has shown the incidence of stroke in children to be about 1.2-13.0 per 100,000. About 50% of those strokes are ischemic. In children, strokes are usually seen in patients with sickle cell disease, heart disease, or known thrombophilia.
Posterior circulation ischemic stroke (PCIS) is uncommon and accounts for 20% of all ischemic stokes in children. PCIS typically affects the cerebellum and brainstem which can result in ataxia, cranial nerve deficits, and crossed hemiparesis. Vertebral artery dissection is the most common cause (50%) for PCIS. In cases of minor trauma resulting in dissection, there can be an associated structural abnormality of the cervical spine.
Due to our patient’s history and clinical exam, there was immediate concern for vertebral arterial dissection. This often presents with ataxia, headache and emesis in children. Neck pain is not commonly seen (~12%). Conventional angiography is the gold standard for diagnosis but is invasive. MRI and MRA have become first line diagnostic modalities because they are noninvasive, have no radiation and can simultaneously diagnose both stoke and dissection.
Our patient’s initial imaging did not reveal a vertebral artery dissection. To further evaluate for vascular and cervical spine abnormalities, a CTA was obtained and it was also normal. Her cardiac ultrasound with agitated saline was normal. Hypercoagulable work up was negative. Inflammatory markers were normal. No etiology could be identified for her PCIS. There have been case reports of vertebral artery spasm as a potential cause for cerebellar ischemic stroke.
Management of ischemic stroke in children depends on the etiology. If there is an extracranial dissection, guidelines recommend anticoagulation. Neurosurgical procedures are also an option for children with dissection who continue to have symptoms despite medical management. If there is not dissection or vascular anomaly, aspirin alone can be given at 3-5 mg/kg. Thrombolytic therapy is not recommended in children. Our patient was medically managed and discharged home on aspirin.
Conclusions: PCIS is rare in pediatrics. When a child presents with ataxia and any focal neurologic findings, stroke needs to be considered. If there is concern for PCIS, then the vertebral artery should be evaluated for dissection. MRI/MRA can evaluate for both dissection and stroke.