Background: Hemorrhagic complications after cardiac catheterization (CC) and percutaneous coronary intervention (PCI) are associated with an increased risk of mortality. In review of a large catheterization registry, blood transfusions were required following 1.4% of radial access and 2.8% of femoral access PCIs, respectively. While there is a standardized protocol for obtaining a blood type and antibody screen (T&S) and transfusion preparation for most surgical procedures at our institution, there is no such protocol for medical procedures. There is evidence from perioperative literature to suggest that in surgical procedures with rates of transfusion of less than 5%, routine pre-operative T&S may be unnecessary. Currently, there is no standard protocol for ordering a T&S prior to inpatient CC at our institution and no nationally accepted guidelines. Our goal was to explore the current practice and assess the cost effectiveness of obtaining routine T&S prior to inpatient CC.
Methods: A retrospective chart review was completed of 331 hospitalized patients who underwent 362 consecutive left heart catheterizations from October, 2016 to April, 2017 at an academic medical center.
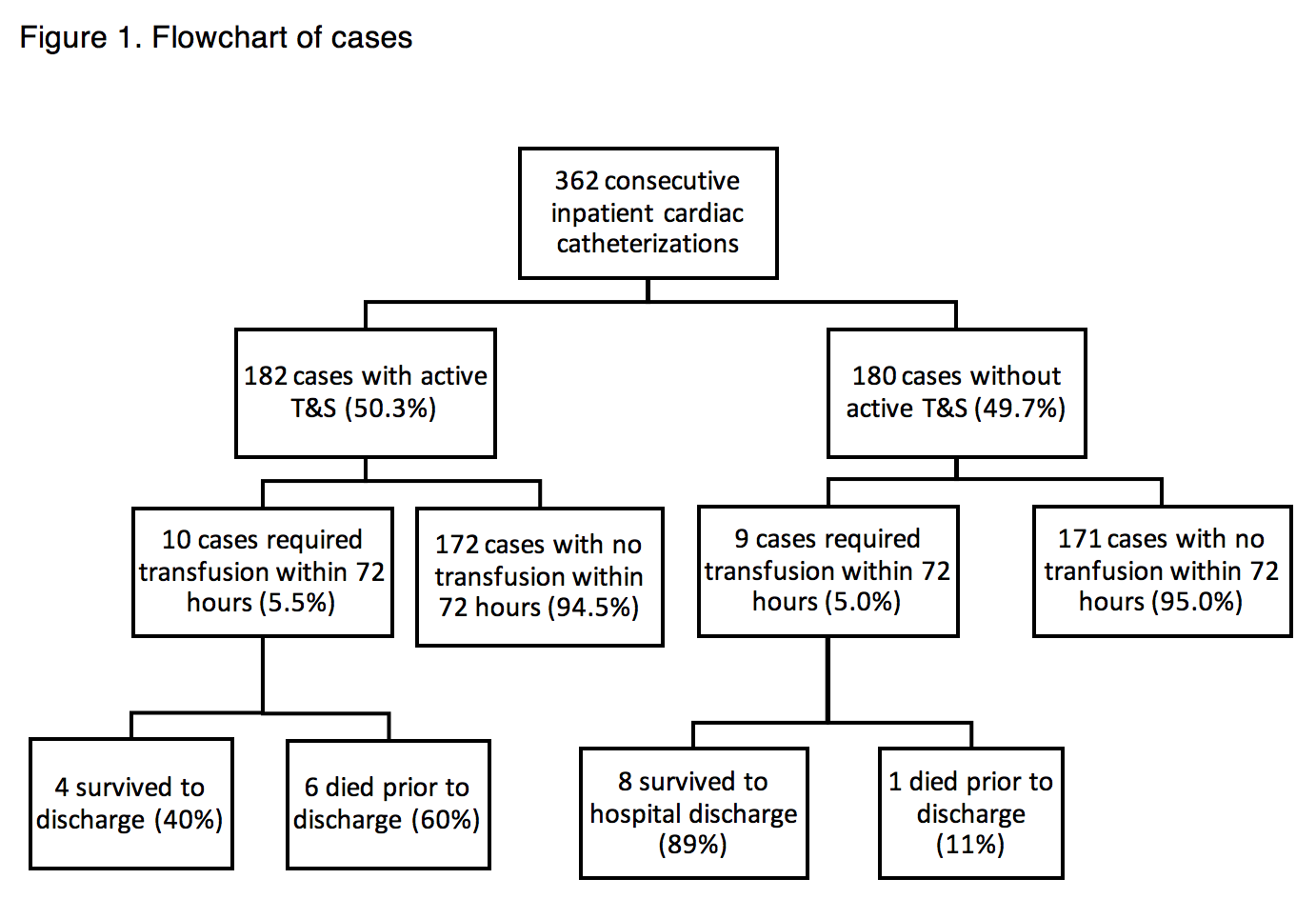
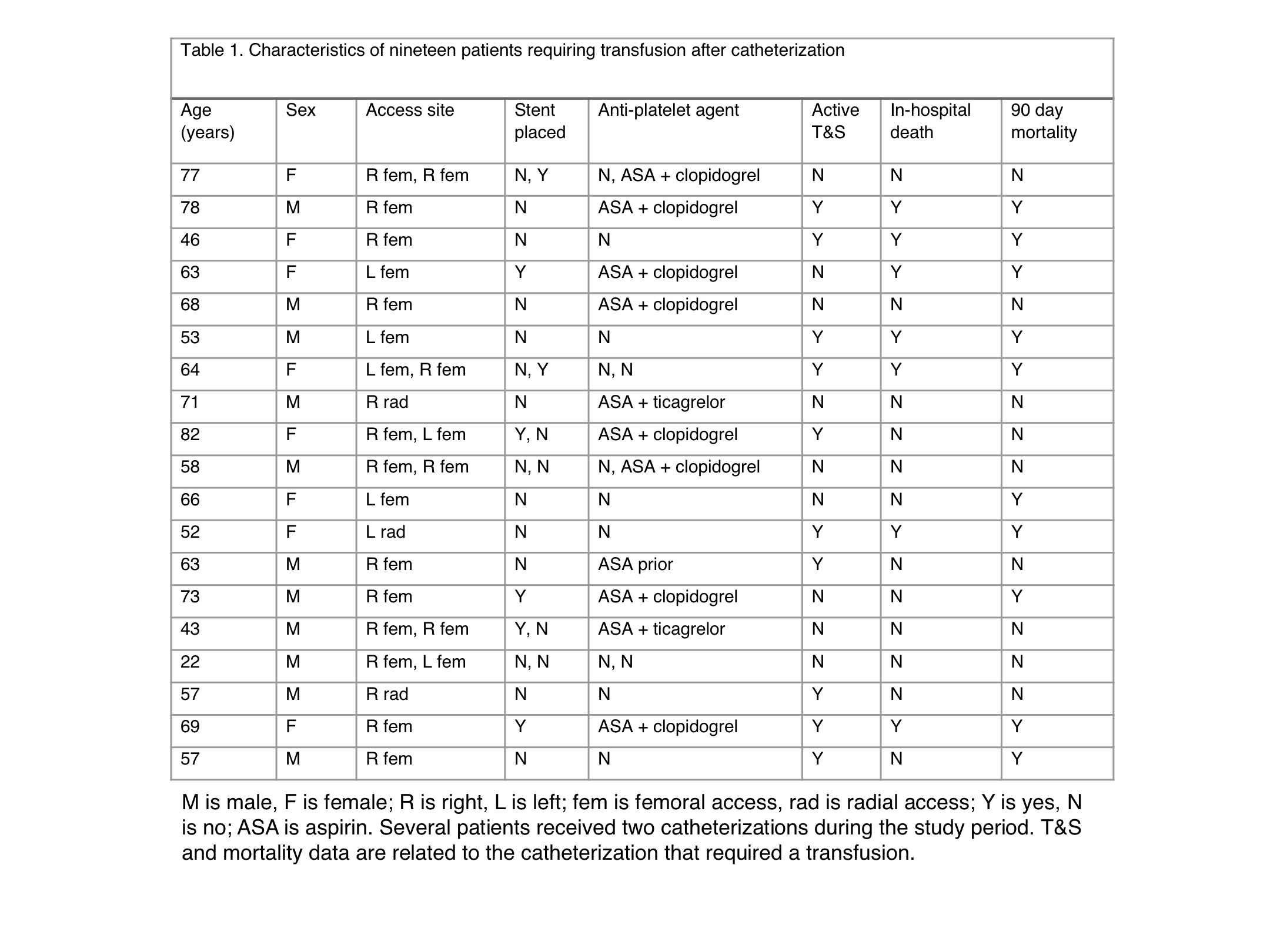
Results: A T&S was active (drawn within 72 hours of procedure) in 180 of 362 (49.7%) inpatient CC cases (Figure 1). There were 19 total patients that required a blood transfusion within 72 hours of CC. Ten of those 19 patients (Table 1) had an active T&S at the time of catheterization. Additionally, nine bleeding complications directly related to CC requiring transfusion out of 362 procedures (2.5%), which is consistent with prior large multicenter published studies. Of the 19 patients that required transfusion, seven died during the admission (36.8%), while ten died within 90 days of catheterization (52.6%). Further, there was a trend towards increased in-hospital mortality among those patients who had an active T&S (p=0.057). Of those nine patients that experienced bleeding complications related to CC, seven (77.7%) survived to hospital discharge.
Conclusions: Our review demonstrated that our transfusion requirement rate following CC is consistent with findings in the published literature. In the current non-standardized approach of routine T&S prior to inpatient CC, less than half of the patients had an active T&S prior to CC. Moreover, there was no clinical benefit for patients with a pre-procedure active T&S and a trend towards increased in-hospital mortality in those with an active T&S, which suggests that we should approach T&S prior to CC in a clinically nuanced manner. Given the relatively low risk of bleeding complications and the ability to rapidly complete a T&S and prepare emergency blood, routine ordering of T&S on all patients prior to inpatient CC should not be recommended. An annual cost savings of $92,672 would be estimated if this policy were adopted at our institution.