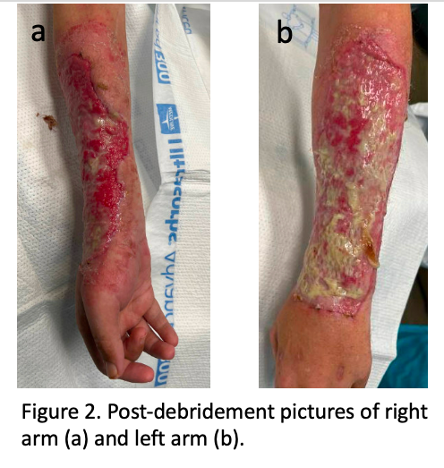
Case Presentation: A 42-year-old male with a history of intravenous (IV) drug abuse presented with four weeks of skin lesions on his bilateral dorsal forearms and one week of associated right-hand swelling and anesthesia. Prior to the development of the skin wounds, the patient had been frequently injecting fentanyl into the veins of both forearms; he was aware that the drug contained xylazine as an additive. He first noted the lesions as small ulcers. Over the next four weeks, the lesions expanded to encompass nearly the entire dorsal surface of his forearms. On presentation, he was afebrile and tachycardic. Physical exam revealed large ulcerative lesions with overlying necrosis on the dorsal aspect of his forearms extending from wrists to elbows (Figure 1). The right hand was swollen with anesthesia of the dorsal surface, but was without erythema, warmth, fluctuance, or pain. Labs were only remarkable for an elevated CRP of 53 mg/L (reference range < 10 mg/L).He was started on empiric IV antimicrobials and admitted to the hospital. Blood cultures were obtained at the time of admission and had no growth. The burn surgery team was consulted and performed extensive debridement of both wounds for definitive source control (Figure 2). Antibiotics were continued through the second debridement (a total of ten days). He had improvement of his right hand swelling, however retained mild range of motion restrictions in the right hand. His hospitalization was complicated by opioid withdrawal for which he was started on methadone.
Discussion: Xylazine is a veterinary drug used for sedation and analgesia. It is a potent alpha-2-adrenergic agonist that decreases the release of norepinephrine and dopamine in the central nervous system, resulting in sedation, muscle relaxation, and decreased perception of painful stimuli.1 Peripherally, the drug causes arterial vasoconstriction. In humans, side effects include bradycardia, hypotension, CNS depression, and respiratory depression.1 It is increasingly being utilized as an additive in illicit drugs, such as heroin or fentanyl, as it lengthens the duration of effects of these otherwise short-acting agents.1 Importantly it is not an opioid and thus does not respond to naloxone. In 2022 approximately 23% of fentanyl powder and 7% of fentanyl pills seized by the DEA contained xylazine.6Xylazine is associated with skin injury, commonly abscesses or ulcers, the pathophysiology of which is thought to be chronic vasoconstricting effect on local blood vessels leading to decreased perfusion and impaired wound healing.2 Typical presentation includes progressive, large painful ulcerations that are often foul smelling.5 Other case reports have noted skin necrosis as well.3,4 The skin damage leaves afflicted individuals with an increased risk for infections, including cellulitis, necrotizing fasciitis, myositis, and osteomyelitis.5 Once diagnosed, blood and skin cultures should be obtained along with consideration of x-ray and MRI to rule out secondary infection. Wound care and debridement, sometimes amputation, are necessary for treatment of xylazine-induced skin injury, along with treatment of any secondary infections.5
Conclusions: Xylazine is has emerged as a growing threat, making some of the already deadliest drugs (fentanyl) even deadlier.6 Hospitalists should maintain a high level of suspicion for xylazine exposure in patients who inject illicit drugs, especially when ulcerative lesions or skin necrosis are observed at injection sites.