Background: With the increasing focus on patient experience over the last decade in American healthcare, it is not surprising that numerous interventions to improve sleep in the hospital setting have arisen. However, measuring sleep in the inpatient setting can be challenging. The majority of inpatient sleep studies have focused in the ICU, primarily using patient-reported measures but some studies employed the more objective polysomnography. In addition, outpatient literature has shown a discrepancy between perceived sleep measures and objective sleep measures. To our knowledge, this association has not been evaluated in the general inpatient population. This study aimed to objectively quantify and describe inpatient sleep and how it relates to patient perceptions.
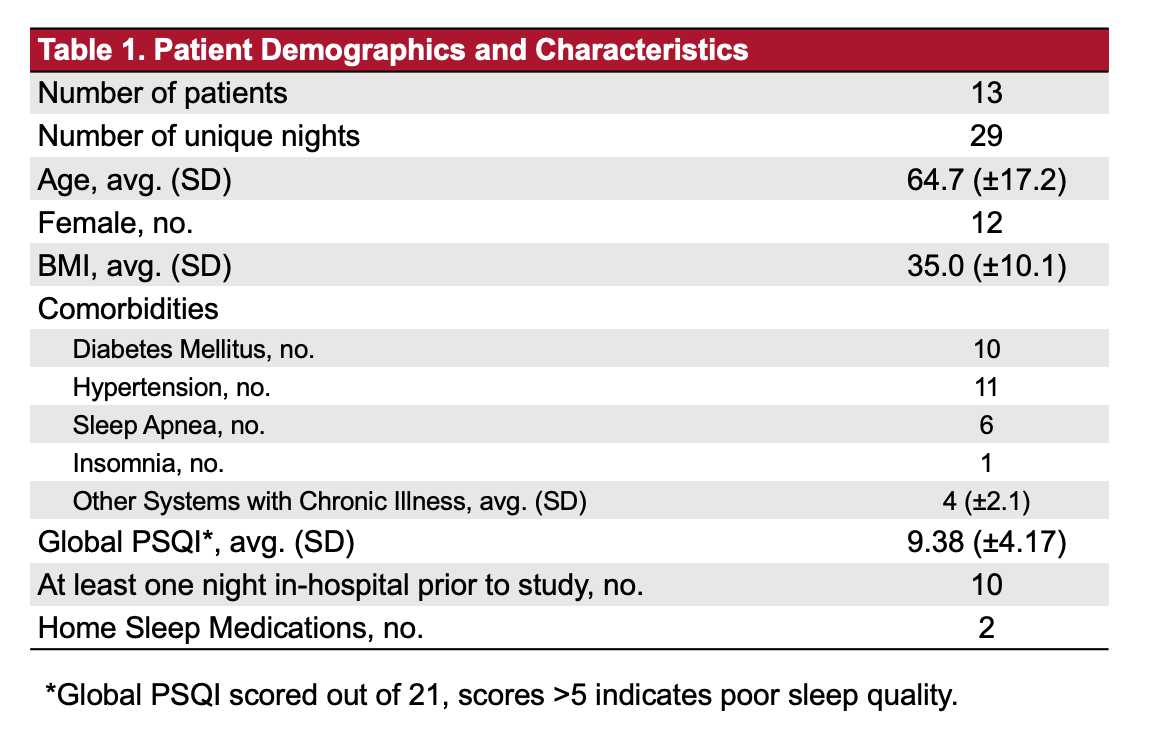
Methods: We conducted a prospective cohort study of patients admitted to the Hospital Medicine service at the University of Nebraska Medical Center. Baseline sleep quantity and quality were assessed using the Pittsburgh Sleep Quality Index. Perceived sleep quantity and quality in the hospital were assessed each day using the Verran and Snyder-Halpern Sleep Scale and by a self-report sleep diary. Daily mood was assessed each day using the Positive and Negative Affect Schedule. Actual patient sleep was measured using wrist activity monitors (ActiGraph wGT3X-BT). Patients completed a patient satisfaction questionnaire on the last day of the study. Chart review was performed to collect relevant patient information.
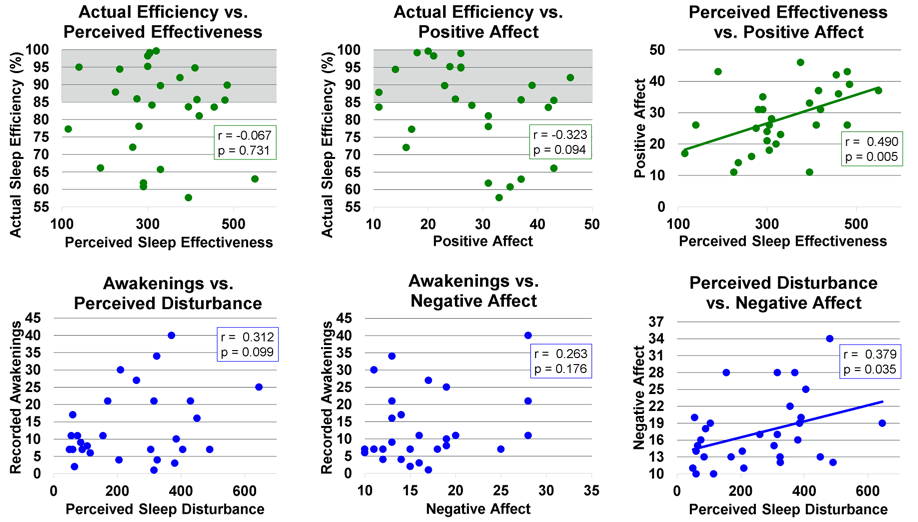
Results: Thirteen patients completed the study with a total of 29 patient nights. Patients were on average 64.7 years old and the majority were female. Other patient demographics are in Table 1. There was no significant relationship identified between perceived and actual sleep efficiency or sleep disturbances (Figure 1). Additionally, perceived sleep time and actual sleep time were not significantly correlated. Actual sleep time, efficiency and awakenings as measured by the ActiGraph were not correlated with positive or negative affect. Actual sleep measures were not associated with daily affect. Perceived sleep measures did correlate with daily mood (Figure 1). Patients who perceived their sleep to be more effective were more negative and patients who perceived more disturbances in their sleep were more negative.
Conclusions: Perceived sleep measures and actual sleep measures were not associated in this study population. However, daily affect was associated with perceived sleep measures but not actual sleep measures. There is cause to be skeptical with self-reported measures of sleep in the inpatient setting. These self-reported measures could be related to confounding factors, such as daily affect. Studies employing objective measures of sleep are needed to better understand any potential relationships between sleep and clinical outcomes.