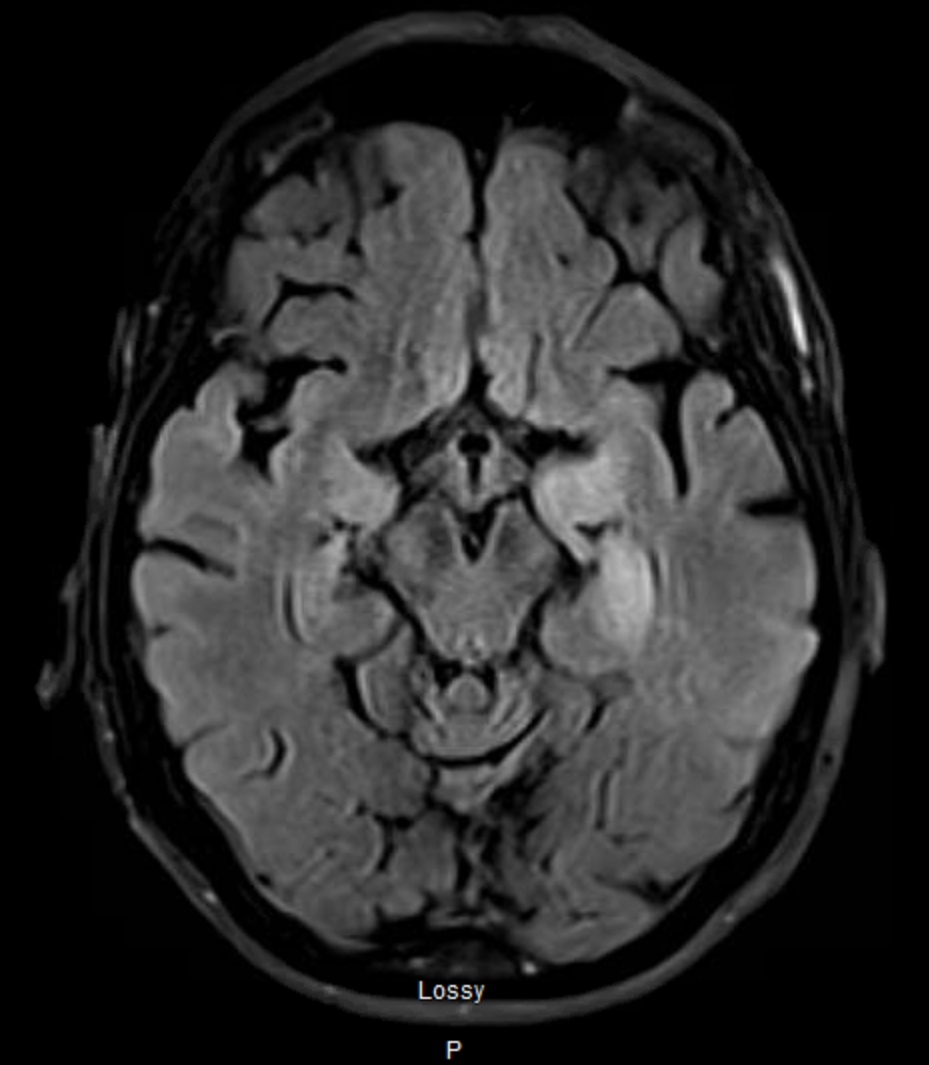
Case Presentation: An 80-year-old female with a history significant for breast cancer status post mastectomy with chemo/radiation therapy and phenytoin-induced liver injury in 2013 presented with nine months of weakness, weight loss, and 2-3 month history of confusion, memory loss, and widespread tremors, suspicious for focal status epilepticus. Workup revealed hyponatremia (135 mmol/L) and elevated LFTs (~40 for both ALT/AST). She underwent treatment in the ED with Keppra, Vimpat, and Onfi, without improvement and subsequently admitted. Continuous electroencephalogram (cEEG) was notable for periodic lateralized epileptiform discharges and subclinical seizure activity originating from the left temporal region. Neurology consult prompted an MRI which demonstrated T2 left mesial enhancement with nodules, suspicious for autoimmune limbic encephalitis. LP confirmed 1:128 titer type 1 antineuronal nuclear antibody (anti-Hu). She received a 5 day course of high dose steroids and 2g/kg IVIG with improvement. To assess breast cancer recurrence, on hospital day (HD)10, a full-body PET scan showed a hypermetabolic mesial temporal lobe and pulmonary nodules. Biopsy was consistent with SCLC and she was discharged on HD12 with plans to titrate medication, follow-up with neuroimmunology, and scheduled chemotherapy/radiation. Post-treatment chest abdomen pelvis CT showed good response. Patient has been managed outpatient for recurrence, neurological symptoms, and prevention.
Discussion: Our findings demonstrate an unusual presentation and diagnosis of pulmonary malignancy. Approximately 1-7.4% of patients with cancer are diagnosed with paraneoplastic syndrome, with SCLC being the most common (1). These syndromes are generally either caused by ectopic hormone production or an abnormal immune response leading to tissue destruction caused by neural antigen expression from cancer cells. The latter can lead to a paraneoplastic neurological syndrome, which affects approximately 3-5% of patients with SCLC (1,2). In this case, the patient’s altered mental status and progressive systemic symptoms along with a history significant for cancer necessitated full workup, which identified a rare etiology of SCLC: limbic encephalitis (LE). LE belongs to a larger, more generalized disease called paraneoplastic encephalomyelitis (PE). An estimated 40-50% of patients with LE are simultaneously diagnosed with SCLC (1). Treatment for LE, caused by tissue damage as a result of onconeural antibodies, is focused on immunosuppression and immunomodulation. Without immediate and ongoing treatment, individuals presenting with neurological signs, including AMS and status epilepticus, hold a poor prognosis (3). Thus, early recognition and intervention is critical to preserve neurologic function and prevent further neurodegeneration.
Conclusions: The aim of this case report is to add to the literature about limbic encephalitis as a presentation of SCLC and to encourage clinicians to consider it in the differential for patients presenting with AMS and systemic signs of progressive disease. A thorough workup is critical to determine disease etiology as well as underlying malignancy.