Background: Team-based approaches have been broadly promoted to improve healthcare delivery in the U.S. However, few studies have analyzed the complexities of team-based communication in the current healthcare delivery landscape of increasing electronic health record (EHR) use and the rapidly evolving EHR functionalities. Major hurdles to studying effective communication within and between healthcare teams include: the expansive scope of this research inquiry; detailed communication data between team members; and rigorous methods to analyze communication data. Based upon the large body of research on network analysis, we explored the application of network analysis to visualize healthcare teams at a large, urban academic medical center with EHR data.
Purpose: Based upon the large body of research on network analysis, we explored the application of EHR access data to describe the connectivity and network structure of healthcare teams at a large urban academic medical center.
Description: The study was approved by its Institutional Review Board. A total of 100 surgical colorectal cancer patients receiving treatment in 2013 and 2014 were selected at random. We used detailed access logs for the Cerner EHR system to create a table of encrypted patient identity, medical record number, users’ identity, clinical position/role of the user, date of access, and several other variables of the access action.
We pulled data from one month before cancer diagnosis to nine months post diagnosis. There were approximately 2.45 million records of access logs. More than 6,800 unique users, representing over 150 roles or occupations, accessed the health records. Decisions regarding exclusion and categorization were reached through consensus of three physician project team members. After excluding student learners and database analysts, we categorized the remaining users into three groups: core patient care team, support team, and administrative team.
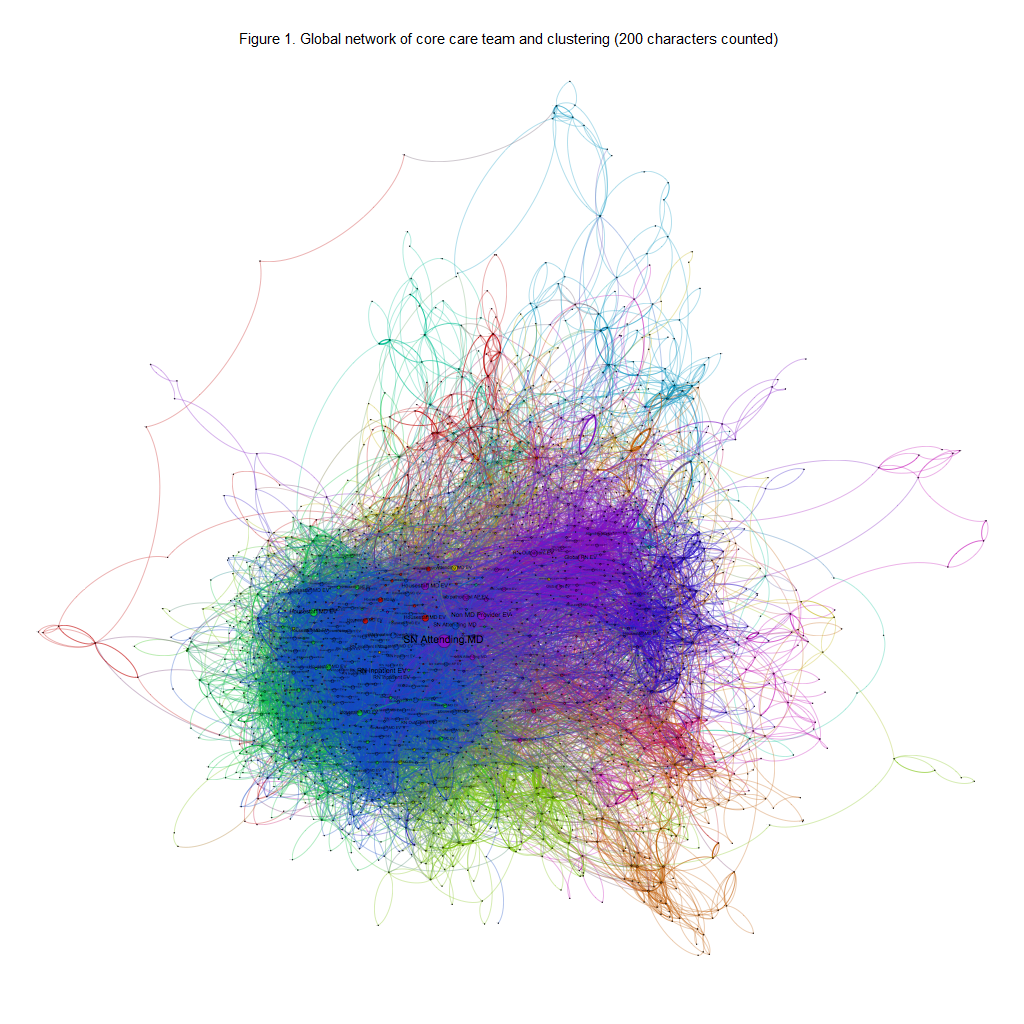
Figure 1 shows the global network of the core patient care team, which depicts regular information transmission ties among core care providers. The network was constructed using 1,933 different providers in the medical center who were connected to an average of 5.8 other providers; however, over 20 of them were very highly connected (>100 other providers). There were 13 subgroups based on the closeness of their relationship. The size of subgroups ranged from 3 providers to 320 providers. The largest subgroup was dominated by inpatient nurses and housestaff physicians, and the second largest subgroup was led by outpatient nurses and attending physicians. The longest path length (i.e., the minimum number of information transmission ties needed to connect two providers) between any two nodes in the network was 14. The average path length was 4.09.
Conclusions: This study demonstrates that EHR systems can provide extensive and detailed data to describe the connectivity and network structure of healthcare teams. Future study is needed to validate this method in studying team care.