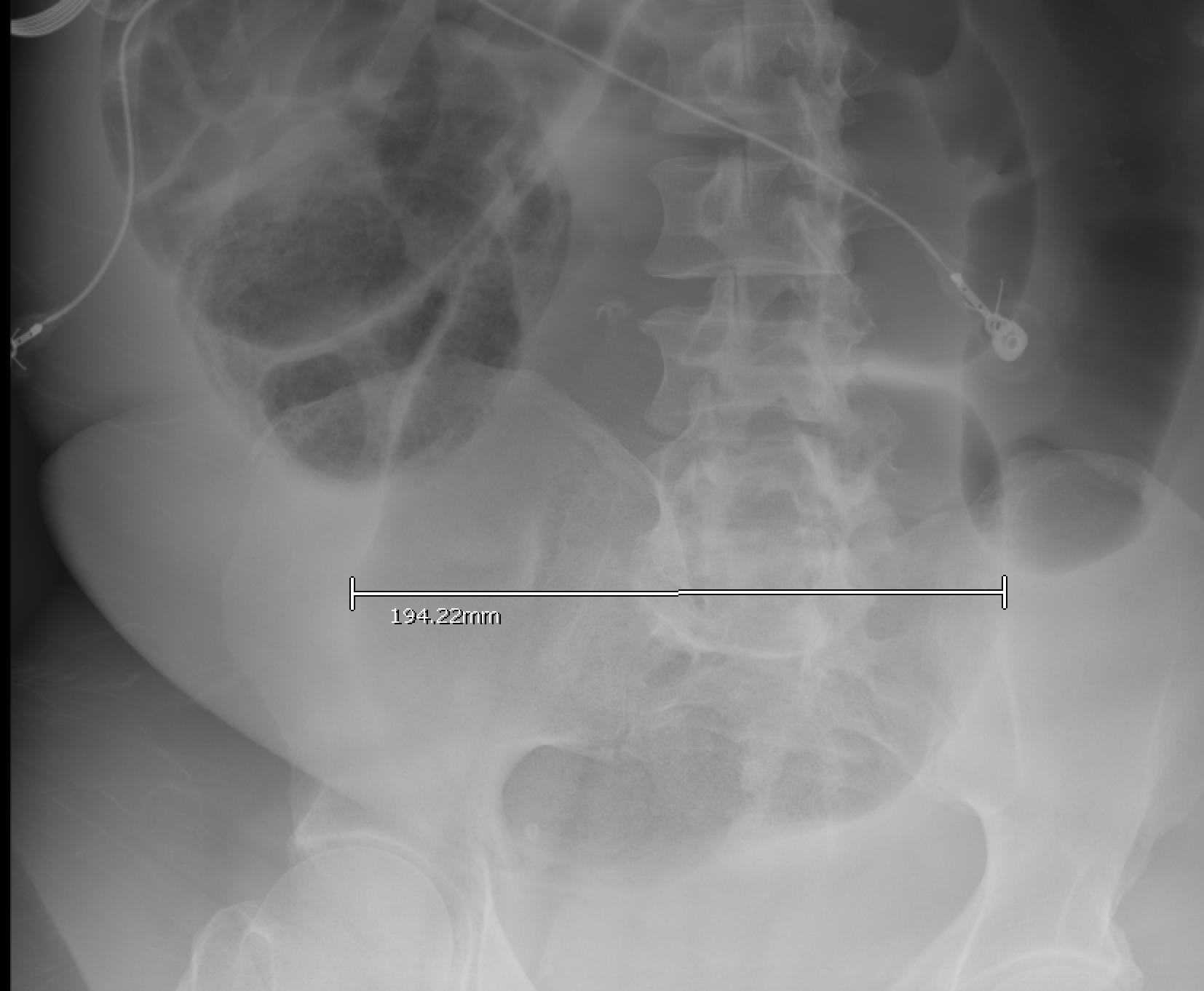
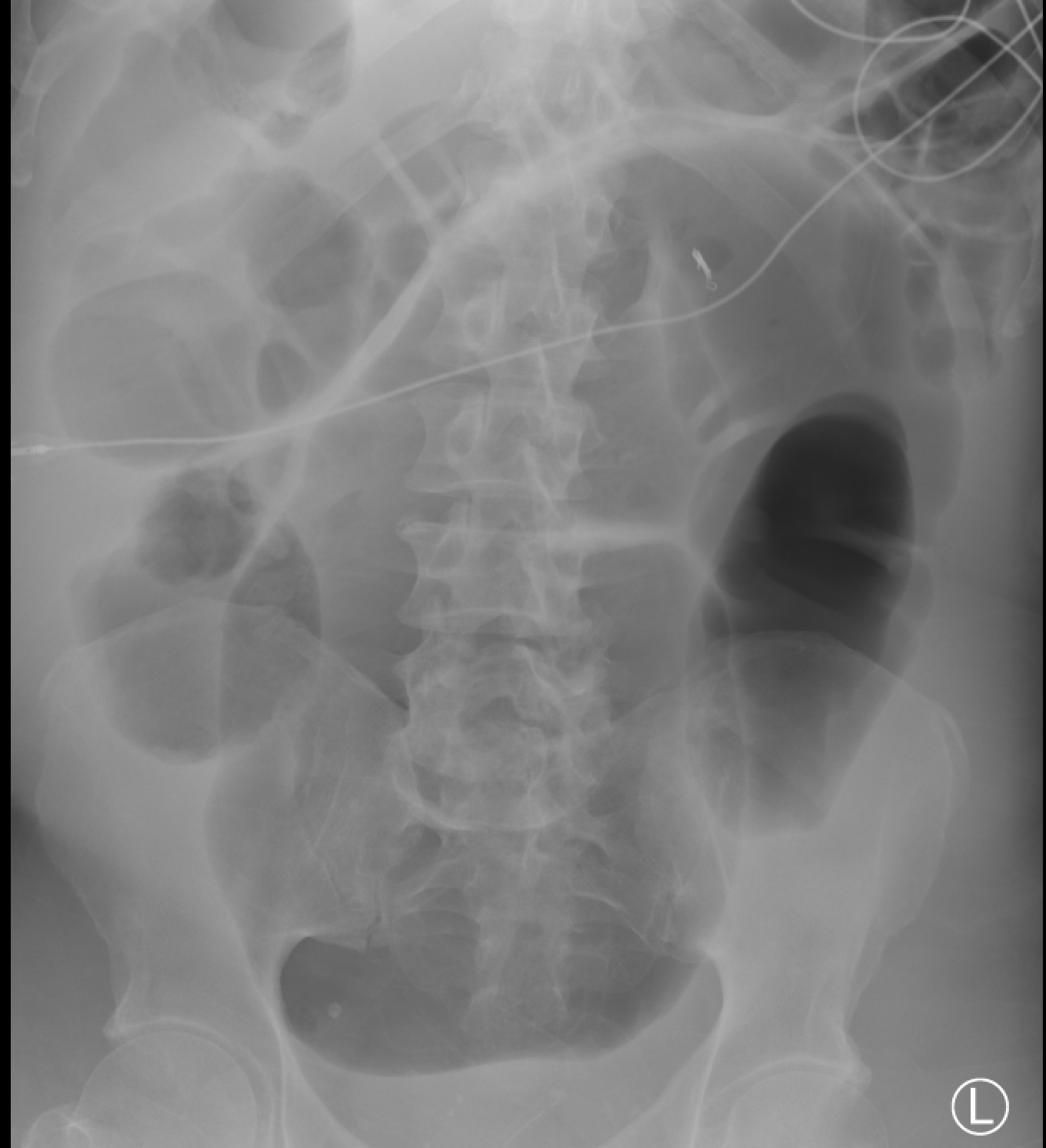
Case Presentation: A 58 year old male with a past medical history of hypertension, hyperlipidemia, diabetes mellitus type 2, and stage 4 chronic kidney disease presented to the ED for 3 weeks of weakness, dyspnea, and bilateral lower extremity edema. Exam and workup was notable for anasarca, albumin of 1.8 g/dL, and CT with ascites and dilated sigmoid colon (Fig 1). He was admitted for workup of anasarca and bowel dilation.He underwent colonic decompression with initial improvement of dilation. Workup for anasarca ruled out heart failure, cirrhosis, or oliguric renal failure. A 24 hour urine collection showed non-nephrotic range proteinuria. He developed hypokalemia to 2.2 mEq/L, with low urinary potassium. Nephrology was consulted and recommended biopsy and spironolactone. The biopsy showed chronic sequelae of diabetes and hypertension.Over weeks of hospitalization, he continued to have small-volume diarrhea, abdominal distention and anasarca. He required 260 mEq of IV and oral K+ repletion daily to maintain an average K+ of 2.7 mEq/L. He developed a non-anion gap metabolic acidosis requiring a bicarbonate drip. The severe electrolyte derangements were attributed to ongoing secretory diarrhea. Imaging noted recurrence of sigmoid colon dilation up to 20 cm (Fig 2). Several doses of neostigmine and repeat colonic decompression yielded transient improvement. The patient was placed on bowel rest and started on TPN. He elected to undergo sigmoidectomy with Hartmann’s pouch formation. Two weeks following the procedure, the patient tolerated a normal diet, his stool solidified, and electrolytes normalized. On day 53 of hospitalization, he was discharged to acute rehab.
Discussion: Our patient was diagnosed with refractory colonic pseudo-obstruction (CPO), or Ogilvie’s Syndrome. He presented with profound colonic dilation and secretory diarrhea (SD-CPO) – a rare, lesser-known presentation (1). This subtype’s severe electrolyte derangements (hypokalemia) are thought to be secondary to dramatic upregulation of colonic potassium channels (1, 2). There is a possible predisposition to CPO in CKD/ESRD, a state in which these receptors are already up-regulated due to CKD (2, 5). SD-CPO is less likely to respond to standard conservative management of bowel rest, neostigmine, and endoscopic decompression (1, 3, 4). Our patient failed these conservative therapies and had significant, recurrent distension with clinically refractory electrolyte derangements, necessitating hospitalization for repletion. He experienced a dramatic resolution of his symptoms only after undergoing sigmoidectomy.
Conclusions: SD-CPO is a rare, difficult to treat subtype of CPO. Our patient had life-threatening potassium losses even with small-volume diarrhea. Failure of conservative management requiring sigmoidectomy proved to be curative, demonstrating that surgical intervention can be used as an effective treatment option in SD-CPO. Moreover, clinicians should be aware of this rare-subtype of CPO as an explanation for refractory hypokalemia.