Background: The COVID-19 pandemic was one of the biggest threats to human health, affecting health and health care delivery systems at both the individual and institutional level. There have been varied reports about how sociodemographic factors affect outcomes of patient with COVID-19 [1] [2] [3]. In this US claims based study, we analysed discharge data for all patients who were admitted for COVID-19 infection in the year 2020 using the National Inpatient Sample (NIS), the healthcare cost and utilization project (HCUP) database of the United States (US).
Methods: Using data from the national inpatient sample for 2020, we evaluated the hospital characteristics of patients admitted with COVID-19 infection in 2020. We used ICD -10 code U071 to assess the rates of COVID-19 infection stratified by age, sex, and race. Using a multivariate model that adjusts for potential confounders, we also evaluated the outcomes (in hospital mortality, respiratory failure, and cardiac arrest) of COVID-19 infection according to age, sex, and race.
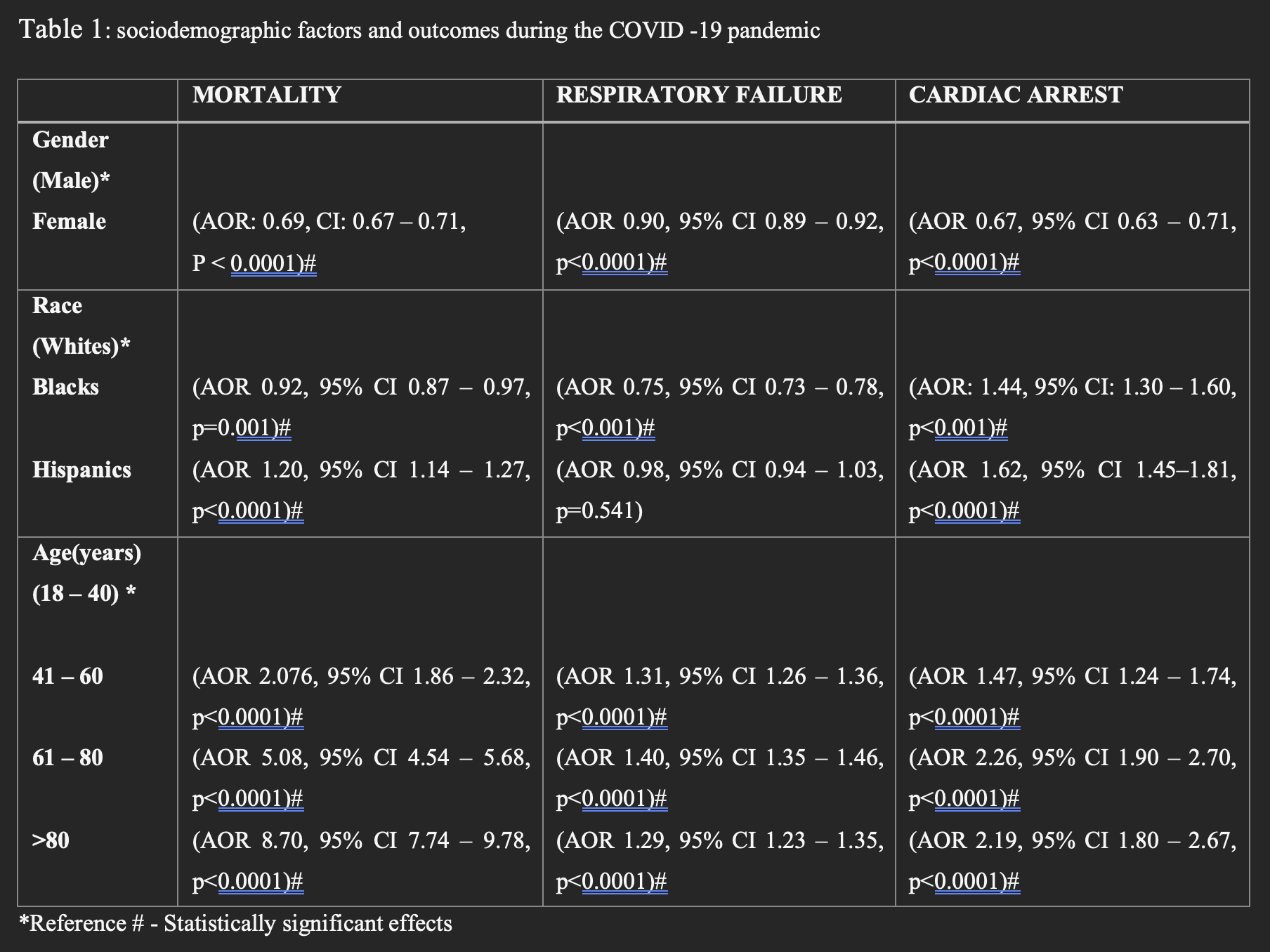
Results: There were 1,050,045 patients admitted for COVID 19 infection during the study period. The proportion of COVID-19 infection was Females (47.2%), Whites (57.5%), blacks (20.1%), Hispanics (22.4%). Admission rates were highest in patients aged 61 to 80 (44.5%). Following multivariate analysis, we observed a lower mortality rate in women (AOR: 0.69, CI 0.67 – 0.71, P < 0.0001). Similarly, they had lower rates of Cardiac Arrest (CA) (AOR 0.67, 95% CI 0.63 – 0.71, p< 0.0001), and Respiratory Failure (RF) (AOR 0.90, 95% CI 0.89 – 0.92, p< 0.0001). Compared to adult patients under 40 years of age, there was an increased chance of mortality in patients aged 41 -60 (AOR 2.076, 95% CI 1.86 – 2.32, p< 0.0001), (61 -80) (AOR 5.08, 95% CI 4.54 – 5.68, p< 0.0001), and older than 80 years (AOR 8.70, 95% CI 7.74 – 9.78, p< 0.0001). Similarly, older age was associated with higher rates of cardiac arrest and respiratory failure. Hispanics had a higher mortality rate (AOR 1.20, 95% CI 1.14 – 1.27, p< 0.0001) and CA (AOR 1.62, 95% CI 1.45–1.81, p< 0.0001) compared to whites, and a nonsignificant association of RF compared to white patients, but black patients, despite having significantly higher CA rates (AOR: 1.44, 95% CI 1.30 – 1.60, p< 0.001), had lower mortality rates (AOR 0.92, 95% CI 0.87 – 0.97, p=0.001) and RF rates (AOR 0.75, 95% CI 0.73 – 0.78, p< 0.001) compared to whites.
Conclusions: Our study shows that patients in the age group more than 60 years, male gender and Hispanic patients all have higher rate of adverse hospital outcomes (Mortality, Cardiac arrest, cardiogenic shock, and respiratory Failure) during COVID-19 related hospitalization. Further detailed retrospective studies with co-morbidities and baseline characteristics stratification are needed to further understand the underlying risk factors and its relation to the higher rate of male and hispanic ethnicity adverse hospital outcomes.