Case Presentation: 43-year-old patient with Down syndrome, intellectual disability and unrepaired atrioventricular canal defect with Eisenmenger syndrome presented with coffee ground emesis and worsening respiratory status. Home medications included metoprolol and folic acid. Patient lived in a foster home and an accurate history was not available. On examination BP was 88/60 mm hg, HR was 107 bpm, RR was 24/min and oxygen saturation at rest was 78% on non-rebreather. Physical examination was significant for clubbing and central cyanosis; chest was clear to auscultation and; cardiovascular examination was significant for a displaced apical impulse and a loud second heart sound. There was trace pedal edema. Chest X ray showed cardiomegaly and prominent central pulmonary vascular markings and peripheral pruning. EKG showed sinus rhythm, RBBB and non-specific ST/T changes, unchanged from baseline. Labwork revealed – Hb 15.1 g/dl, platelets 154 K/uL, leucocyte 9.8 K/uL, BUN 67 mg/dl, Creatinine 0.9 mg/dL, potassium 5.1 mmol/L and sodium 139mmol/L, HOC3 19 mmol/L. Hospitalist team was notified for admission. Review of patient’s outpatient records showed baseline hemoglobin (Hb) was 22 g/dL and baseline oxygen saturation was 85-88%. Acute blood loss anemia from a likely gastrointestinal source was suspected due to a history of coffee ground emesis. Patient received 2 units pRBCs. EGD with cardiac anesthesia showed a bleeding duodenal ulcer that was cauterized. Following blood transfusion oxygen saturation increased to his baseline value of 85% within 48 hours. Increased NSAID use was noted to be responsible for duodenal ulcer.
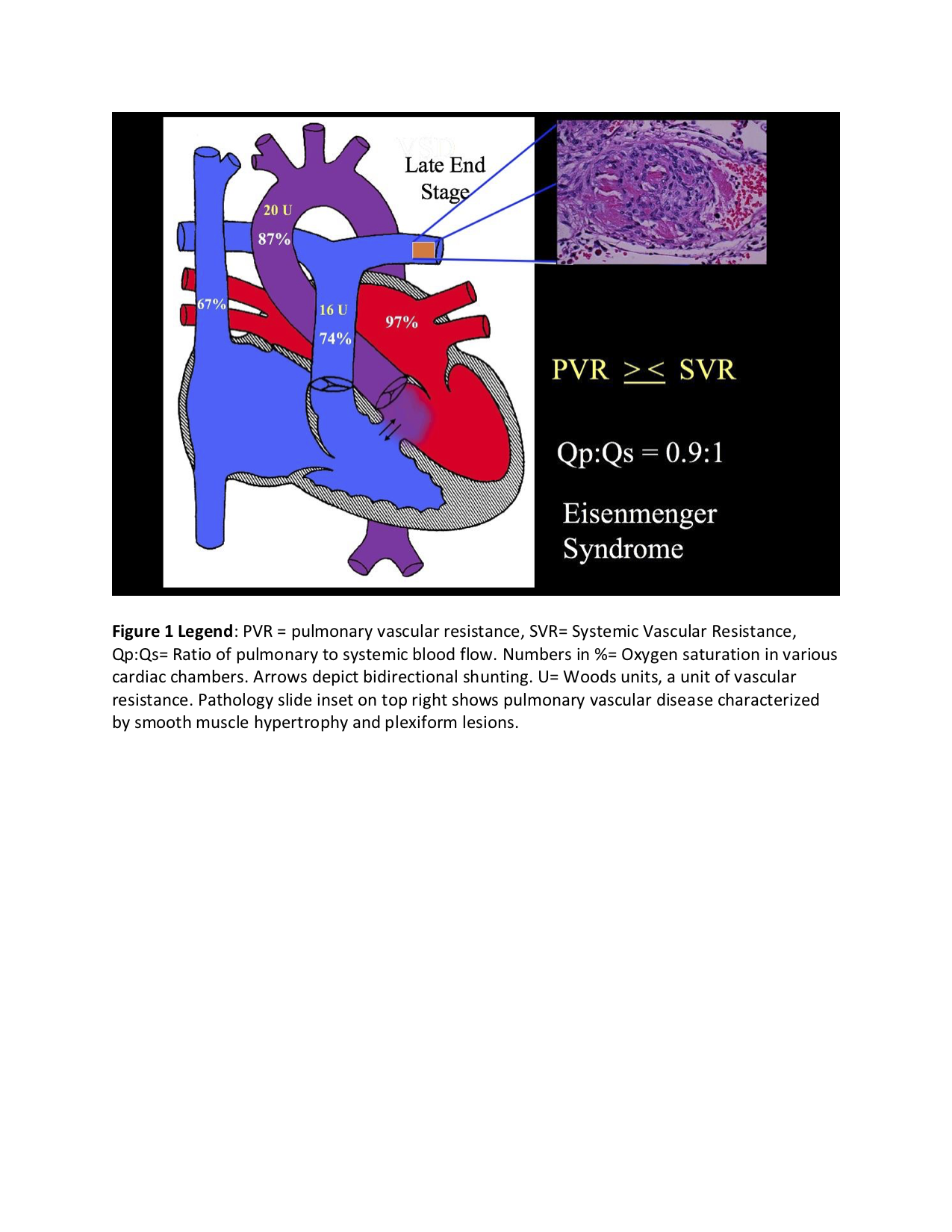
Discussion: Eisenmenger syndrome is a type of cyanotic congenital heart disease in which there is reversal of a large longstanding left to shunt due to development of pulmonary vascular disease. This leads to right to left and bidirectional shunting that causes hypoxemia. Chronic hypoxemia leads to secondary erythrocytosis and an elevated baseline Hb. Degree of erythrocytosis depends on degree of hypoxemia and baseline Hb values of 19-22 mg/dl are not uncommon. Acute blood loss anemia can cause hypovolemia and anemia both of which can cause severe hypoxemia and tissue hypoxia in patients with Eisenmenger syndrome. These factors along with ensuing metabolic acidosis can cause decreased systemic blood pressure and increased pulmonary vascular resistance, thereby increasing right to left shunting and further worsening hypoxemia and tissue hypoxia. Correction of hypovolemia and anemia promptly improved clinical status in our patient.
Conclusions: As Eisenmenger syndrome patients have secondary erythrocytosis, hemoglobin is high at baseline. In this scenario severe blood loss anemia can be missed. Careful attention to baseline hemoglobin can help avoid this error. Hemoglobin must be adequate to the degree of cyanosis. Hypovolemia can be life-threatening by worsening right to left shunting in these patients.