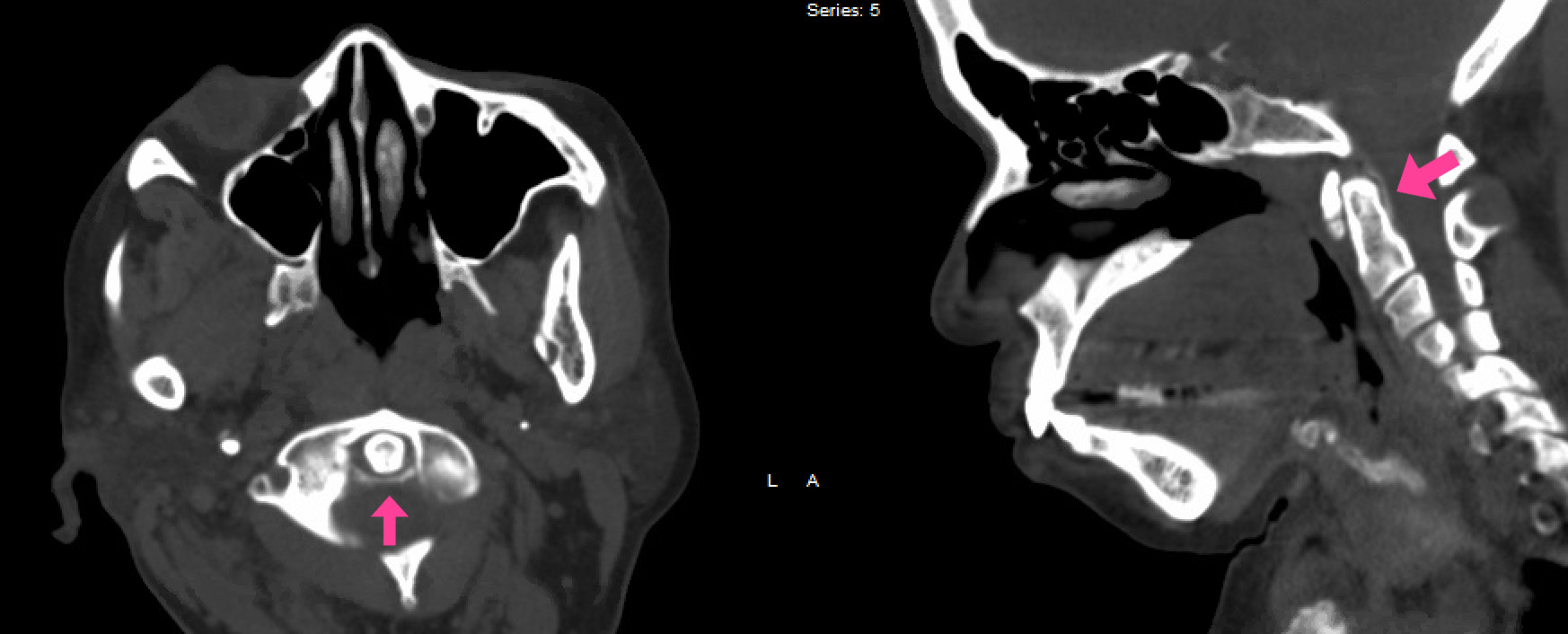
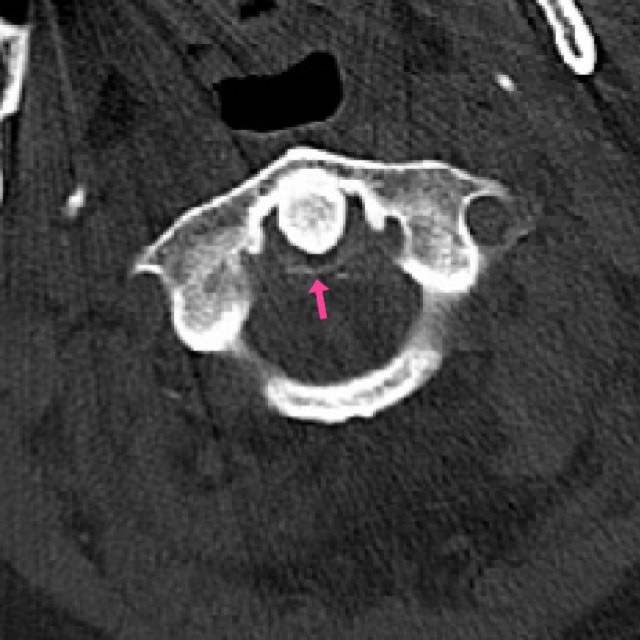
Case Presentation: A 66-year-old female with a history of Cerebrovascular accident, diabetes, hypertension, chronic kidney disease, and osteoarthritis, presents to the hospital for worsening acute neck pain which had woken her up in the night a week prior. She had had minimal to no relief with Tylenol or Flexeril and her neck pain had continued to intensify radiating to the shoulder girdle, leading to marked immobility. Upon evaluation, she exhibited decreased range of motion in the cervical spine with significant limitations in rotation, and no evidence of meningeal irritation. Labs showed elevated erythrocyte sedimentation rate (ESR) >140 mm/hr (0.0-20.0) and C-Reactive Protein of 22.8 mg/dL (0.0-0.9), with no leukocytosis. CT of the cervical spine showed chondrocalcinosis of the transverse ligament of the atlas (Fig.1). Given her sudden onset severe cervical pain with stiffness, imaging, and elevated inflammatory markers with no evidence of infectious etiology, Crowned Dens Syndrome (CDS) was suspected. She was treated with methylprednisolone 40 mg followed by 20 mg the nest day in addition to Colchicine 1.2 mg once and 0.6mg daily for prophylaxis. The next day she reported dramatic improvement in her pain and range of motion, which further supported the suspected diagnosis. In outpatient clinic, her labs had normalized and she had complete resolution of her symptoms.Two weeks later a 73-year-old female with a history of coronary artery disease, heart failure recently on diuretics, hypertension, and osteoarthritis presented with sudden onset shoulder pain and fevers. On day two of admission, she woke up with severe neck pain and stiffness with no signs of meningeal irritation, which prompted further workup. She was found to have an elevated ESR >140 mm/hr (0.0-20.0) and CT cervical spine revealed retro-dental ligamental calcification (Fig.2). She was started on NSAIDs and methylprednisolone with improvement in her symptoms followed by Oral prednisone for 5 days on discharge.
Discussion: Crowned dens syndrome is a rare form of calcium pyrophosphate dihydrate deposition disease. It is characterized by acute onset severe neck pain resulting in restricted neck rotation, which is associated with calcification deposited in the transverse and alar ligaments surrounding the odontoid process 1. The predilection for crystal deposition in and around the dens leads to the hallmark “crown-like” pattern seen on imaging2. In the acute form, there is an inflammatory response with elevated acute phase reactants with or without fever, oftentimes provoking clinicians to pursue workup for meningitis or Inflammatory arthritis. Females are more commonly affected, and risk factors include older age, osteoarthritis, CKD, and diuretics2.
Conclusions: According to a study by Sayed Ali, et al, there have been 35 reported cases of Crowned Dens Syndrome, however the exact incidence remains unknown, with recent literature proposing that CDS may be more common than previously documented1. Patients respond well to corticosteroids, colchicine, and NSAIDs, therefore CDS is often treated symptomatically without formal diagnosis. It is important to consider Crowned Dens Syndrome in elderly patients who present with sudden onset neck pain accompanied by restricted motion, radiologic evidence of CPPD deposition surrounding the dens, and elevated inflammatory markers in the absence of infectious etiology. In doing so, extensive workup such as intrusive lumbar punctures, an extended hospital stay and incorrect treatment can be avoided.