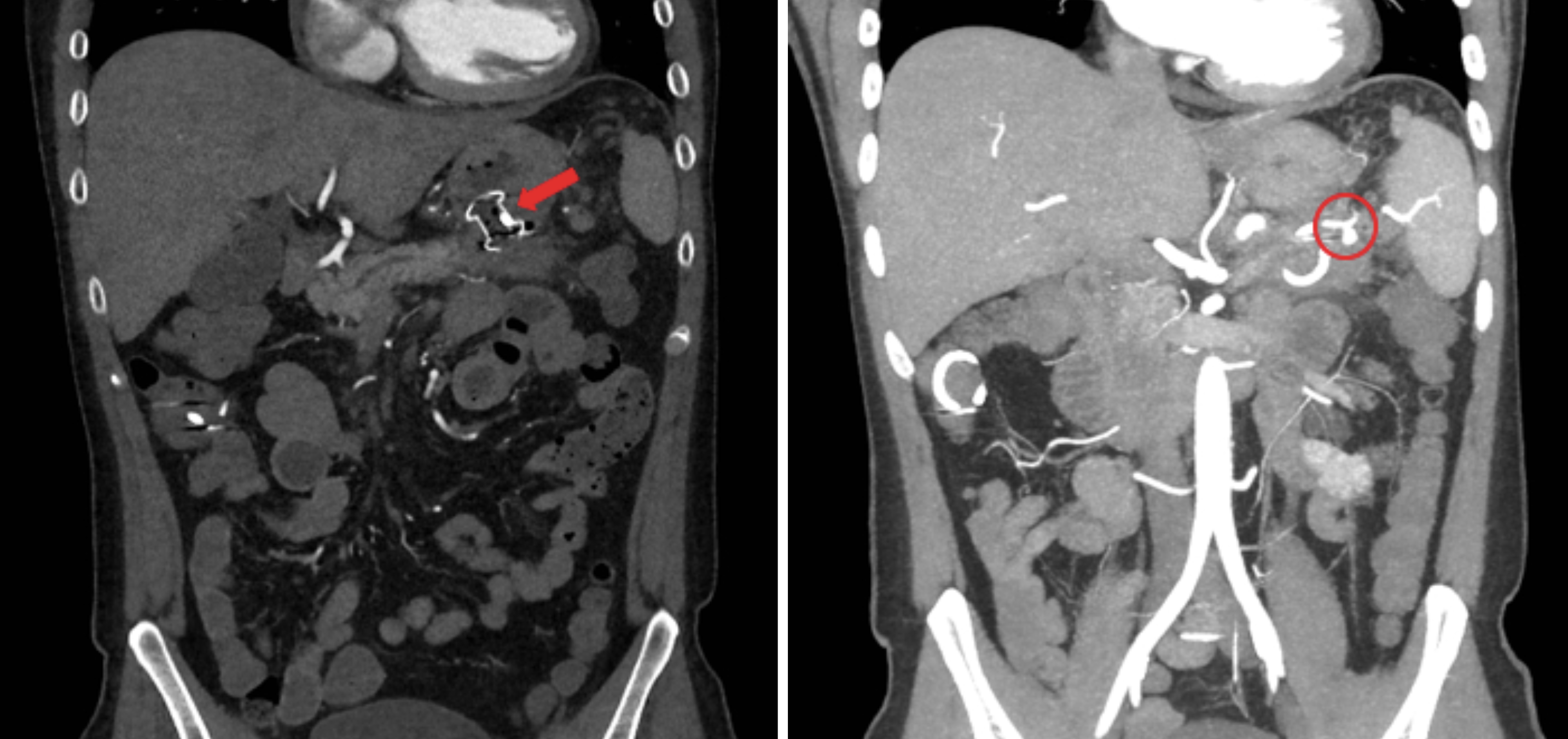
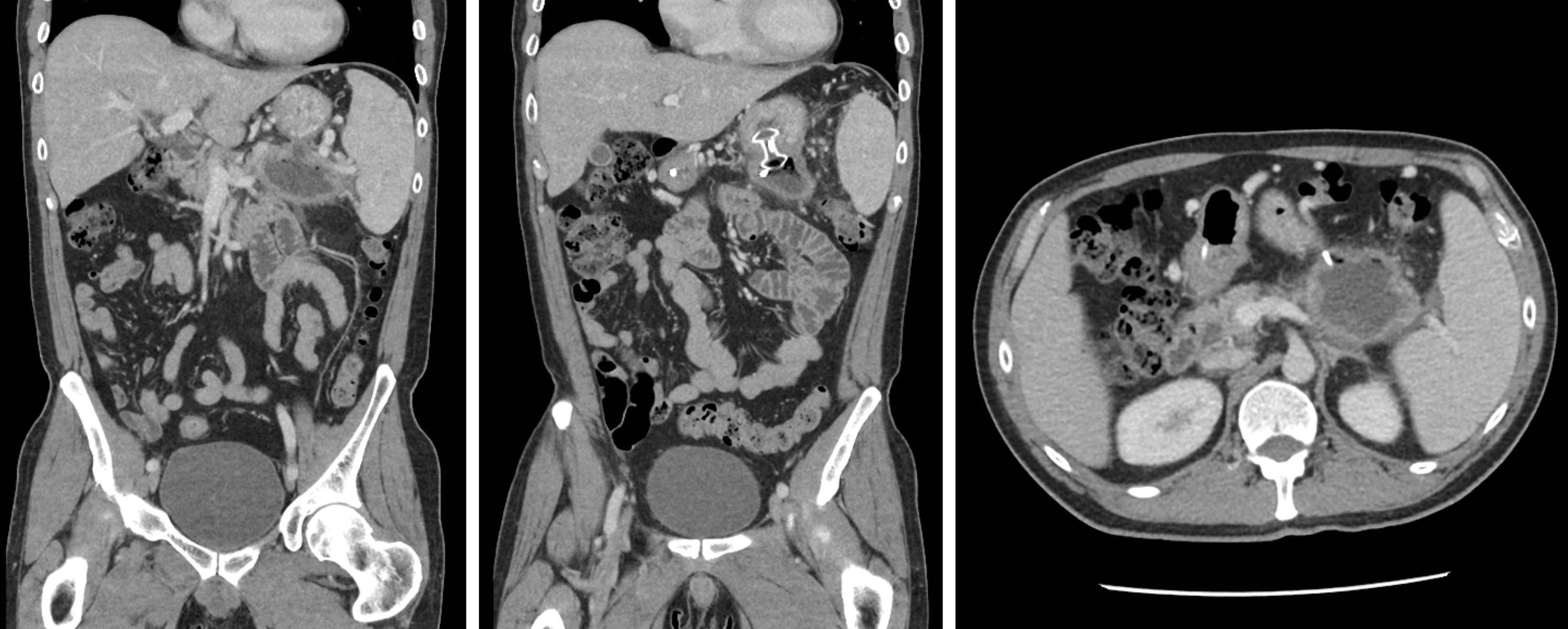
Case Presentation: A 45 year-old gentleman with a history of recurrent alcoholic pancreatitis complicated by pancreatic pseudocyst presented to the hospital after three episodes of hematochezia. Ten days prior, he had undergone endoscopic transgastric metal stent placement between his pseudocyst and stomach, followed 6 days later by pseudocyst drainage with necrosectomy. After 3 days, he then developed nausea, abdominal pain, orthostasis, and hematochezia, so re-presented to the hospital. His heart rate was 106, temperature 99.5, and blood pressure 117/79. He had hyperactive bowel sounds and tenderness to palpation in his left upper quadrant. Laboratory evaluation revealed a hemoglobin nadir of 5.4 g/dL from 9.5 g/dL a week prior at the outside hospital. CT Aorta imaging revealed a 7mm saccular pseudoaneurysm arising from a branch of the splenic artery. Coil embolization of the splenic artery hilum was performed by Interventional Radiology. Complete proximal occlusion of the splenic artery was achieved with no residual aneurysm filling and with resolution of his hematochezia.
Discussion: Chronic and recurrent pancreatitis are conditions frequently encountered by internists. Most common complications include endocrine insufficiency, pseudocysts, and biliary obstruction. A splenic artery pseudoaneurysms (SAP) is an uncommon, but potentially catastrophic, complication of chronic pancreatitis resulting from the weakening of the splenic artery tunica media and adventitia secondary to pancreatic enzyme digestion. SAPs typically present with acute-onset abdominal pain, new anemia, and gastrointestinal bleeding in a patient with chronic pancreatitis—if ruptured, hemorrhage can occur into a pseudocyst, the stomach, pancreatic duct, peritoneum, or retroperitoneum. The location of bleeding dictates the signs and symptoms that develop, such as hematemesis, melena, and abdominal, chest, or flank pain. Although SAP is frequently diagnosed with CTA or MRCP, Angiography is considered the gold standard as it allows for the concomitant therapeutic modality of transcatheter embolization. Splenic artery pseudoaneurysm has been misinterpreted as a cystic lesion on MRCP, raising the potential for inappropriate aspiration and ensuing hemorrhage. All SAPs are considered high-risk for hemorrhage, and there is no demonstrable correlation between pseudoaneurysm size and probability of rupture. As such, surgical treatments are recommended for all SAP lesions. Transcatheter embolization is typically considered the first line intervention and involves the placement of coils proximally and distally to the pseudoaneurysm. As coil embolization carries a 20% risk of reperfusion, yearly screening imaging should be considered. In complex, high-risk surgical cases, alternative interventions such as embolization of the entire splenic artery, partial/total splenectomy, or pancreaticoduodenectomy may be indicated.
Conclusions: Splenic artery pseudoaneurysms are rare, but potentially fatal, lesions that require a high index of suspicion. This case reminds us to include splenic artery pseudoaneurysm on the differential diagnosis for hemodynamic instability in patients with chronic pancreatitis.