Background: Hospitalists are key stakeholders in patient flow throughout the hospital and are pivotal in creating efficient patient movement. Throughput metrics are a large focus for all hospitals, and it takes collaborative effort from many disciplines to effectively shift patient flow toward efficiency.
Purpose: To reduce decision to admit to bed minutes in a collaborative way, using a new workflow concept for ED physicians, hospitalists, logistics and floor nursing staff.
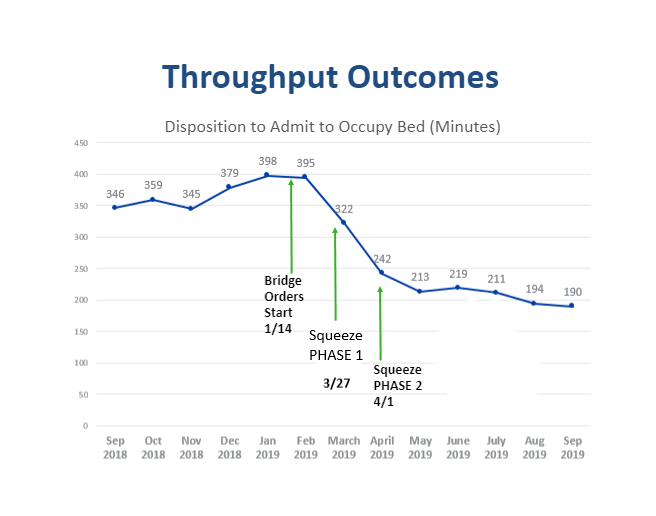
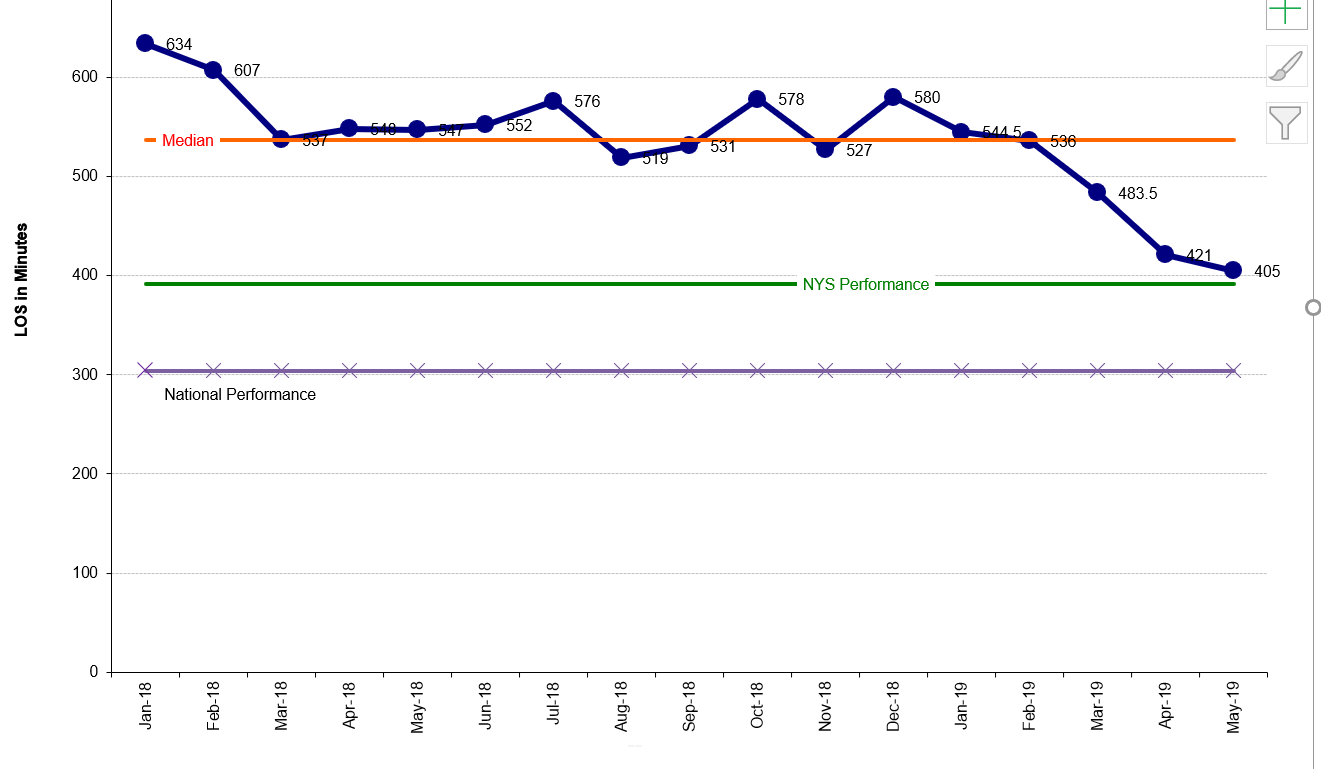
Description: Huntington Hospital targeted ED arrival to bed occupancy for strategic improvement in 2019. Baseline, admit decision to bed occupancy neared 400 minutes. Hospitalists were charged with sparking an initiative that would decrease time substantially. The first iteration of attempts to improve flow looked at barriers to patient movement. Bridge orders were implemented to move the patients from the ED to the floor while awaiting admission evaluation in an effort to move waiting patients from ED areas. This decreased disposition to bed time by 40-80 minutes. It also opened the door to a culture of change for providers, nursing, and logistics.After implementing bridge orders and sparking a readiness for organizational change, the squeeze concept was introduced. It was known that patients were coming. It was also known that the patient flow was dependent on hand off from ED provider to the hospitalist, duration from sign out to admission orders, and again the time from orders to bed arrival. The capacity of the ED was viewed as a full sponge and moving toward a preemptive squeeze of the sponge would be more efficient to offset that capacity. Using this “squeeze” mindset, we implemented changes.The first phase of the squeeze involved nursing. Once orders (admission or bridge) were placed, logistics assigned a bed and notified the floor. Traditionally, ED nurses would have to call report to the floor prior to patient transport. The squeeze concept shifted responsibility to the floor nurse to make calls to get report and then call transport, squeezing the patient from the ED to their assigned bed. This reduced time of placement to bed by ~50 minutes. It also created a more collegial relationship between floor and ED nurses by shifting focus to patient centered care rather than prior adverse interactions. The second phase of the squeeze was implemented with ED providers and hospitalists. By factoring in patterns of clustered patients and targeting end of shift sign outs, hospitalists identified 2 key times to squeeze admissions from the ED. Rather than waiting until end of shift admissions, the admitting doctor sought out admissions that were pending labs or imaging but otherwise met criteria for admission. The admitting physician then distributed to rounding teams to help offload the ED. This decompression was before 5 pm, allowing the day team enough time to round and discharge but not hospitalists end of shift. This intervention impacted not only the disposition to admit orders, but also the door to decision time as well and moved overall throughput metrics down another 80 minutes. By September 2019, throughput metrics averaged 190 minutes, down from 398 at the start of the project.
Conclusions: Applying the squeeze technique showed ~50% reduction in time from decision to admit to placement in a bed. Allowing multiple stakeholders to have ownership of patient flow led to increased teamwork across disciplines. Hospitalists were able to provide the springboard for the collaboration through willingness to approach throughput via an alternate approach.