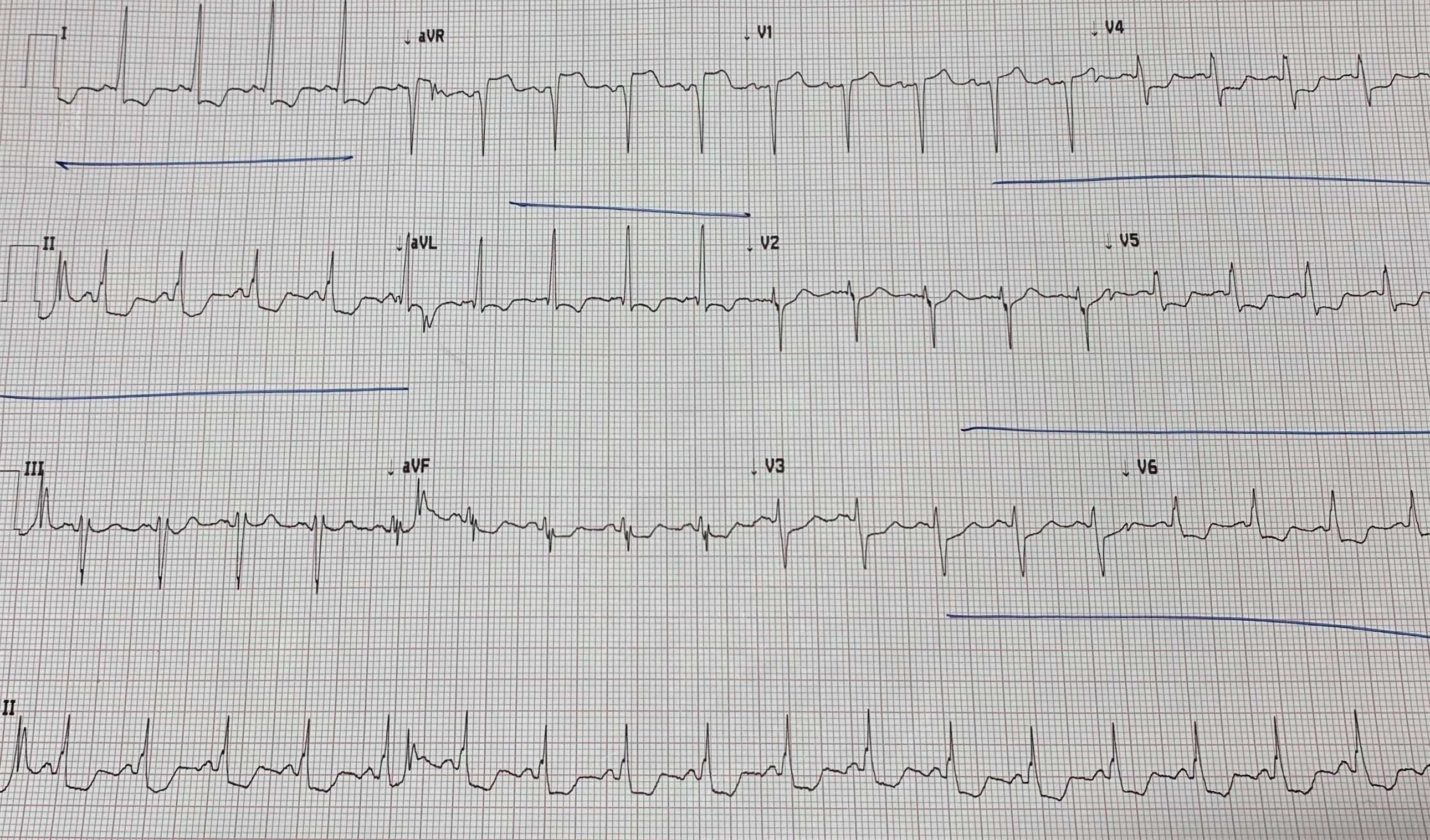
Case Presentation: A 57-year-old man with stable ischemic heart disease presented to the emergency department with stable exertional chest pain. On arrival, the patient was chest pain free and vital signs were within normal limits. Electrocardiogram revealed ST elevation in aVR with ST depressions in leads I, II, and V4 – V6. The patient received loading doses of aspirin and ticagrelor however, in the setting of a negative troponin and a lack of recurrent chest pain, emergent left heart catheterization was deferred. The following day the patient reported new-onset chest pain at rest and was taken immediately for cardiac catheterization which revealed severe triple-vessel disease without evidence of acute occlusion. An intra-aortic balloon pump was placed due to refractory chest pain. Subsequent troponin I was 124 ng/ml and transthoracic echocardiogram revealed a left ventricular ejection fraction of 30%. The patient underwent uncomplicated staged percutaneous coronary intervention and was discharged on hospital day seven.
Discussion: Patients presenting with isolated ST elevation in aVR and multi-lead ST segment depressions are traditionally considered to be at high risk for acute occlusion of the left main or left anterior descending artery. These conditions typically lead to transmural infarction of the interventricular basal septum causing ST elevation in aVR. In tandem with diffuse ST depressions, ST elevations in aVR may be concerning for proximal occlusion in the proper clinical setting. However, recent evidence suggests that acute coronary occlusion is relatively uncommon in patients with these electrocardiogram findings, occurring in only 10% of patients compared to 60-80% in patients with ST elevations in other electrocardiographic distributions. These same electrocardiogram findings are more commonly seen in severe multivessel coronary disease, as a result of diffuse subendocardial ischemia and reciprocal elevation in aVR as seen in this case. Although less commonly associated with acute plaque rupture, patients with these findings are at high risk for future cardiac events. Rates of myocardial infarction, heart failure, and mortality have been found to be higher in patients with ST elevation in aVR, with greater elevation associated with excess risk. ST elevation in aVR is not commonly associated with acute plaque rupture but does indicate high risk for cardiac morbidity.
Conclusions: Current cardiology practice guidelines state that isolated ST elevation in aVR with multi-lead ST segment depressions may represent acute occlusion of the left main or proximal left anterior descending artery. However, recent evidence suggests that the incidence of acute coronary occlusion in these cases is relatively low. Despite low rates of acute occlusion, these patients are at high risk for future coronary events. Although these patients may not need to be taken for angiography emergently, invasive coronary evaluation in a timely fashion is often warranted.