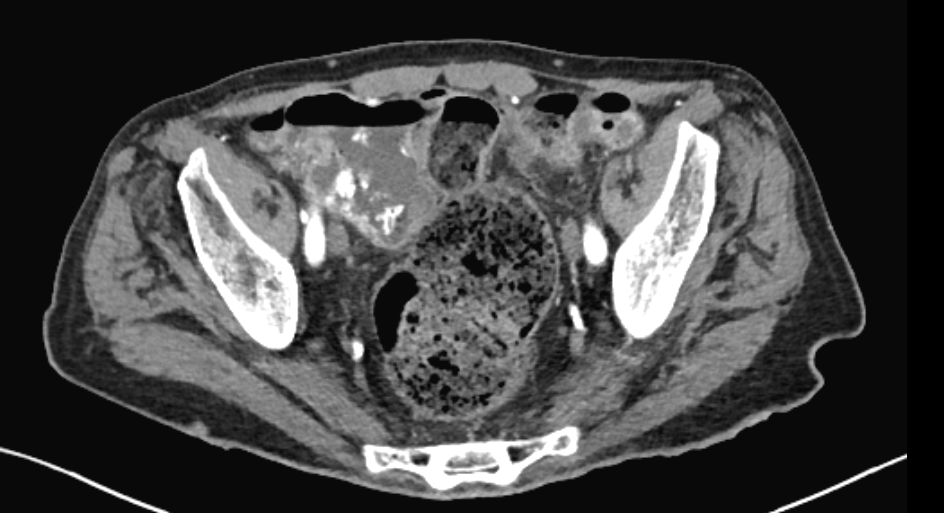
Case Presentation: A 78-year-old man with heart failure, chronic kidney disease, and hereditary spastic paralysis was hospitalized with hyperkalemia to 7.7 mmol/L. He was admitted a month prior with heart failure and discharged on lisinopril with a new prescription for spironolactone. The patient had decreased appetite, limited oral intake, mild nausea, and no vomiting with 1-2 bowel movements daily. His exam revealed normal vital signs and was otherwise unremarkable. Labs were significant for a pre-renal acute kidney injury. An EKG showed prolonged PR, QRS, and QTc intervals with no peaked T waves. He was treated with calcium gluconate, insulin and 5% dextrose, furosemide, normal saline, and one dose of patiromer. A chest X-ray was suggestive of pneumonia, but without fever, respiratory symptoms, or a white count, antibiotics were not administered. On hospital day 3, the patient no longer had symptoms, but his white count increased from 6.4 to 16.3 cells/µL. On hospital day 4, he complained of nausea and mild abdominal tenderness. He was afebrile with a normal exam; his labs revealed a white count of 32.7 but a normal potassium, BUN, creatinine, and EKG. On hospital day 5, he was started on bisacodyl since he had only one bowel movement since admission. His white count increased to 34.1 with negative blood cultures, normal urinalysis, and improvement of CXR. An abdominal and pelvic CT scan revealed a sigmoid colon and rectum distended with retained stool and pericolonic infiltration consistent with stercoral colitis without free air, abscess, or perforation. Bowel movements were induced with senna, docusate, polyethylene glycol, and magnesium citrate. His white count initially decreased to 18.5 on hospital day 6 and normalized by hospital day 7. He remained asymptomatic and was discharged in stable condition.
Discussion: Stercoral colitis, an uncommon diagnosis, occurs when constipation causes colonic distension that can restrict blood flow and increase susceptibility to ischemia, necrosis, ulceration, and perforation.1,2 Risk factors for this diagnosis are similar to those of constipation in general; in this patient, likely contributing factors included advanced age, nursing home residence, poor oral intake leading to dehydration, hospitalization, and spastic paralysis. The condition may present with abdominal tenderness, and CT scan of the abdomen and pelvis with intravenous contrast is an invaluable diagnostic imaging modality.3 When complications arise, management includes antibiotic administration and urgent surgical consultation with mortality in such patients reported to be as high as 60%.4 This is the first reported case of a patient with stercoral colitis presenting with pronounced leukocytosis in the absence of severe complications. Rapid resolution of leukocytosis following bowel movements with negative blood cultures, urinalysis, and CXR supports the premise that the patient’s stercoral colitis was the cause of his elevated white count.
Conclusions: This is a unique case of a hospitalized patient with stercoral colitis causing pronounced leukocytosis that promptly resolved following defecation. While this is a rare presentation of stercoral colitis, it is an important consideration in hospitalized, elderly patients with limited mobility. Early diagnosis allows for intervention that can prevent mortality and deleterious complications.