Background: Length of stay (LOS) is an important quality indicator and has significant financial implications and impact on hospital throughput. Geriatric Fracture Center (GFC) is a co-management program between Hospital Medicine and Orthopedic for patients who are age 60 and above with fragility fracture. Delays in skilled nursing facility (SNF) rehabilitation placement are a major contributor to prolonged length of stay, especially for GFC where patients’ mobility and functional abilities are significantly impacted. Nearly all patients in GFC require surgery and subsequent rehabilitation. The traditional SNF rehabilitation placement process includes multiple steps: (1) identification of the need for rehabilitation, (2) decision to pursue placement, (3) provision of the application paperwork by a social worker to the patient and family, (4) submission of paperwork to the placement office and various facilities, and (5) awaiting a bed offer from a facility.
Purpose: The purpose of the pilot study was to test viability as well as effect on LOS of early initiation of the SNF rehab placement process via pre-prepared, conveniently available, and user-friendly paperwork folders.
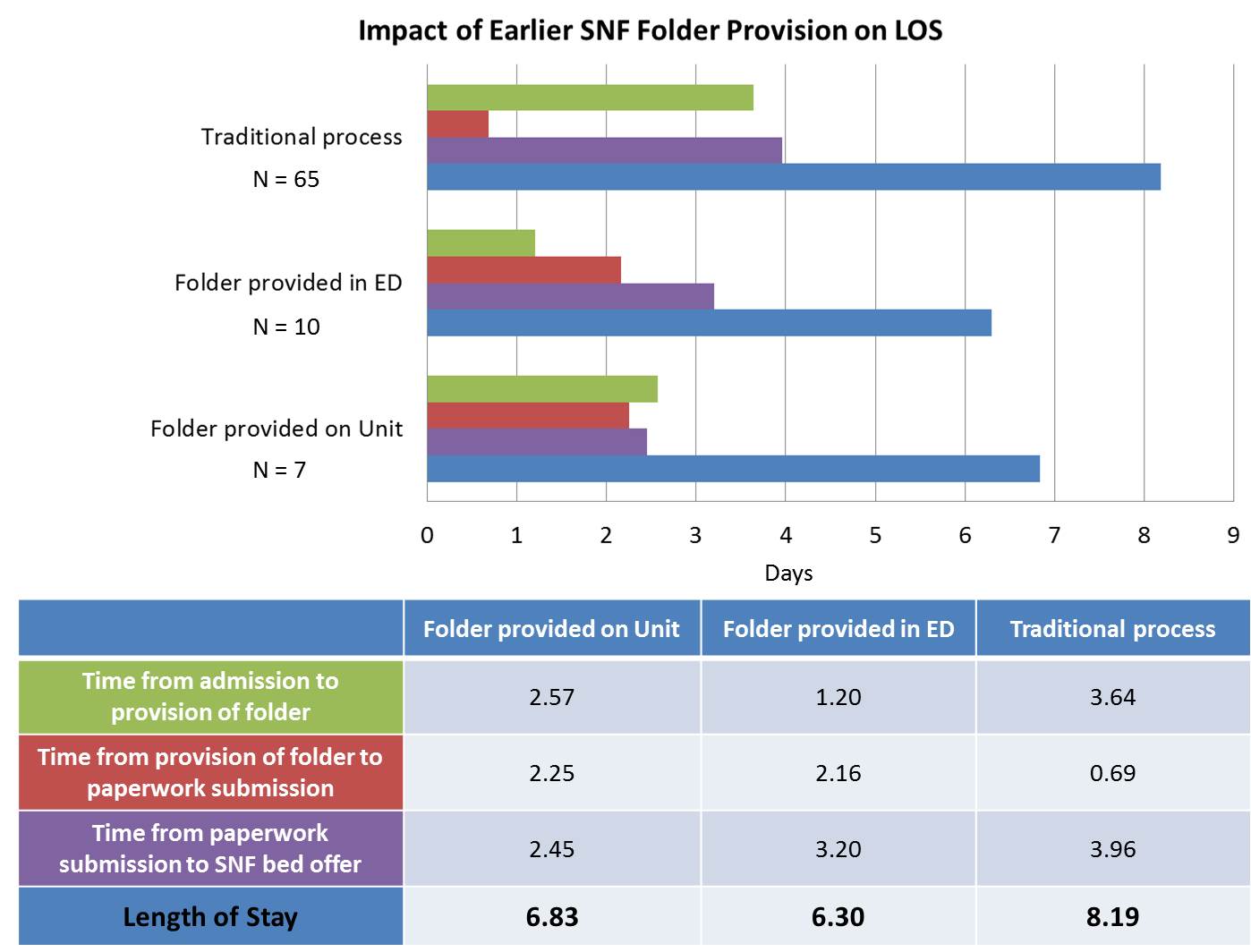
Description: A pilot study was implemented in collaboration between Hospital Medicine, Orthopedics, and Social Work. SNF rehabilitation placement paperwork was assembled into folders and placed in the orthopedic resident work room in emergency department (ED) as well as the orthopedic unit where majority of GFC patients were admitted. Orthopedic residents were provided with a talking script and instructed to provide these folders to patients’ families at the time of consenting for urgent surgery if they predicted SNF rehabilitation placement afterward would be necessary. Nursing and other providers on the unit could also provide the folders to patients and families. We performed a chart review to track the intervals of time from (1) hospital admission to provision of the folder to the patient and family, (2) provision of the folder to submission of completed paperwork to the placement office, and (3) return of the completed paperwork to bed offer from facilities and discharge. Total LOS was tracked. Data from the pilot intervention were compared to the traditional placement process where social workers initiate the process. Average LOS was 8.2 days for the traditional process, 6.3 days when folders were provided through the pilot process in the ED and 6.8 days when received after arrival to the unit (Figure 1).
Conclusions: Initiating the SNF rehabilitation placement process earlier in the admission during the surgical consent process was associated with a quicker turnaround time and decreased LOS. The user-friendly folder allowed non-social workers to initiate the process whenever opportunities arise and streamlined the process.