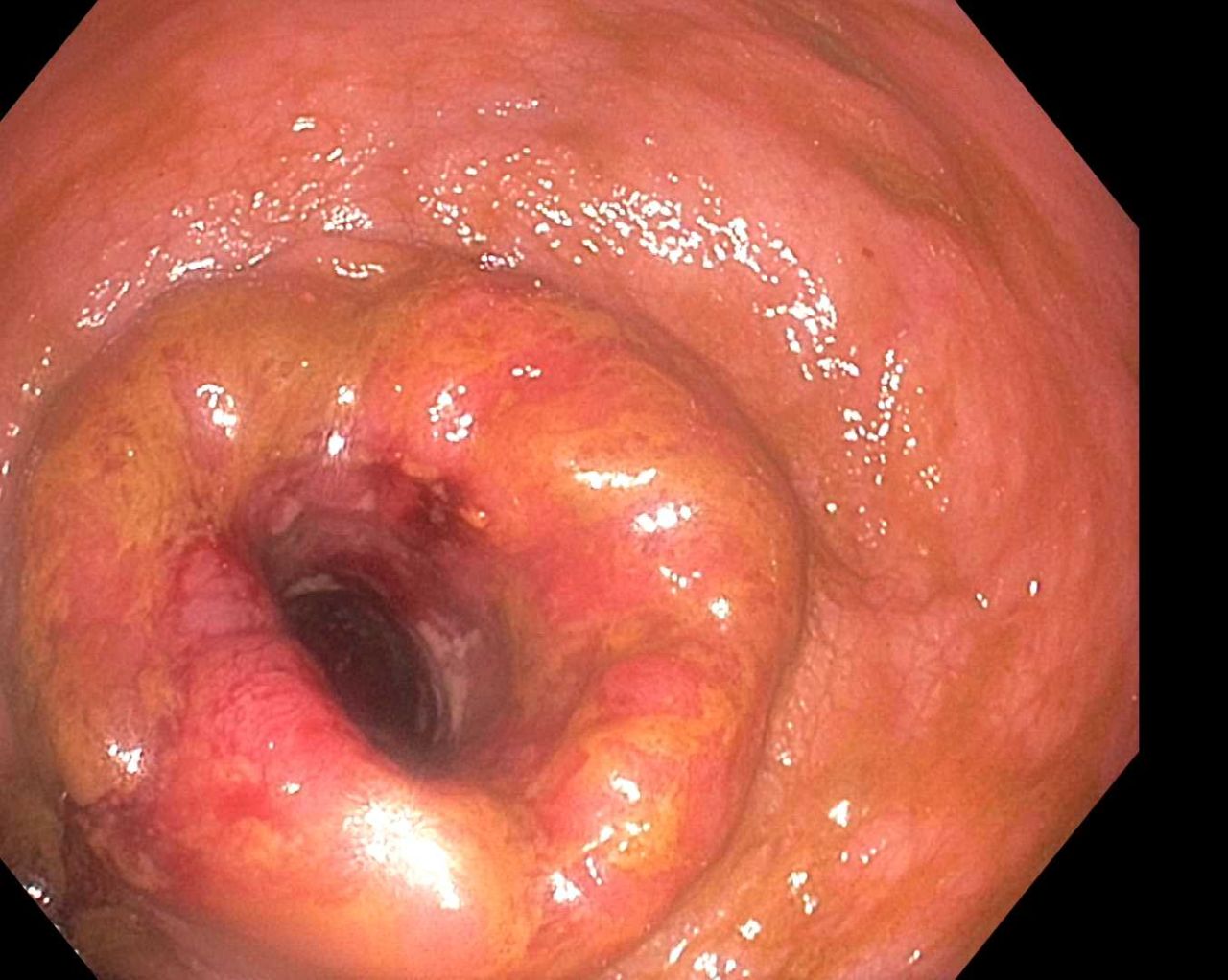
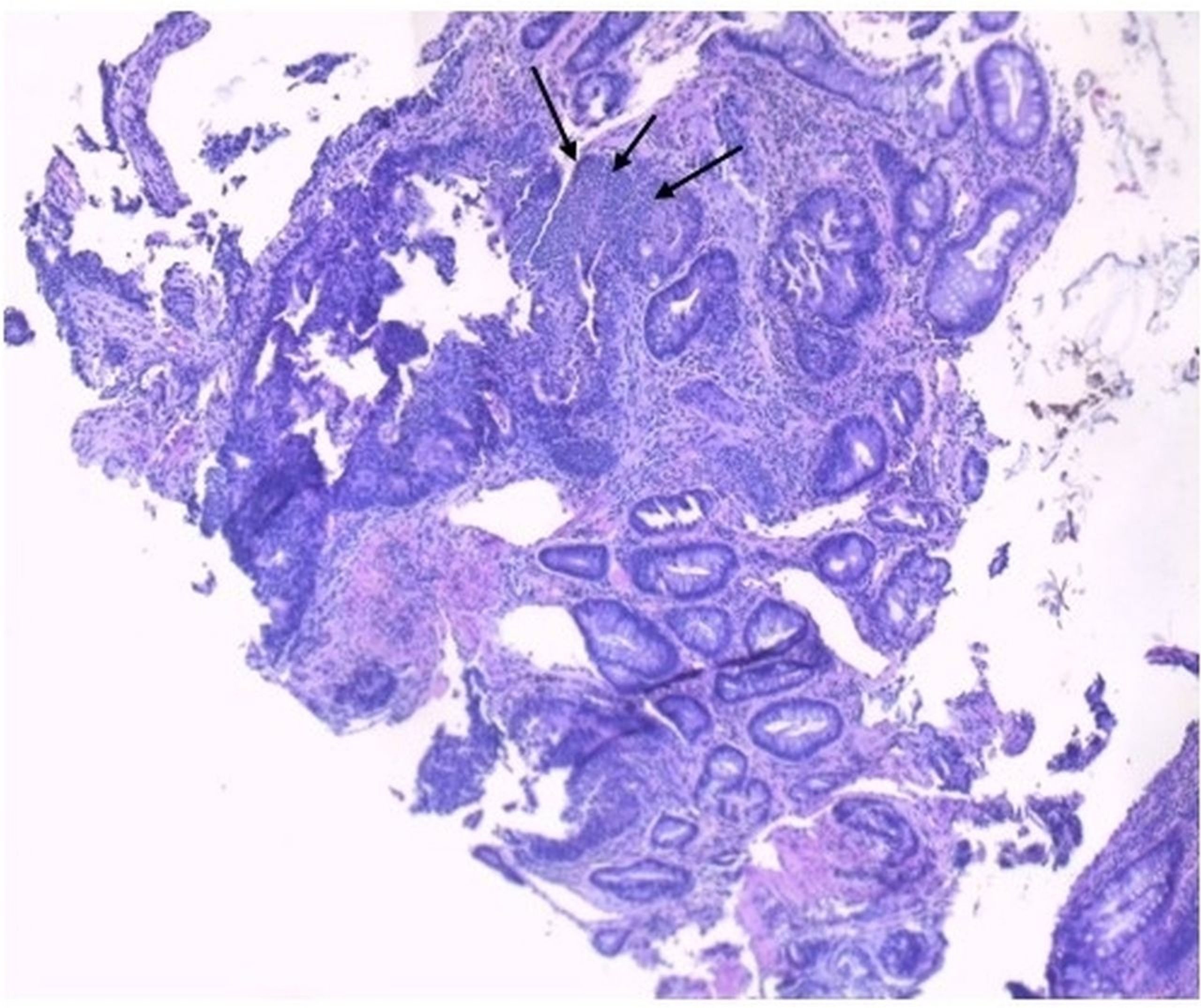
Case Presentation: A 54-year-old female presented with abdominal pain and bloody diarrhea for three weeks associated with fever, chills, nausea and multiple bouts of vomiting. On exam, she was hemodynamically stable and had left lower quadrant abdominal tenderness. Laboratory studies were significant for a left shift with a normal white blood cell count. Her chest X-ray was negative. However, her abdominal computed tomography scan showed a thickening of the left colonic wall consistent with sigmoid colitis without any associated colonic masses or diverticulosis. The blood cultures obtained from two different peripheral sites grew Group A streptococci. The search for the original site of infection was initially unrevealing as the patient’s throat culture was negative for Group A streptococci and a thorough examination did not disclose evidence of skin lesions. The patient was started on an intravenous course of appropriate antibiotics. Based on her findings, a colonoscopy was performed which revealed a large circumferential ulcerative mass at the rectum that impeded further advancement of the scope. The biopsy of the mass revealed a stage III adenocarcinoma of the rectum. Biopsy of the adjacent mucosa displayed features of acute colitis without overlapping features of chronicity which made inflammatory bowel disease unlikely. Surprisingly, the stool culture was positive for Group A Streptococci instead of the common culprits for bacterial dysentery such as Salmonella, Shigella, Campylobacter, and Escherichia coli O:157: H7. This indicated that the primary gastrointestinal infection perpetrated the overt bacteremia. She successfully completed antimicrobial therapy for the bacteremia that lead to negative subsequent blood cultures.
Discussion: Group A streptococcal (GAS) bacteremia from an underlying primary gastrointestinal (GI) infection is very rare. GI symptoms can occur as part of a systemic process with the GAS infection developing elsewhere, most commonly skin and the throat. While GAS perineal disease is common in children, its occurrence in adults is quite rare. Descriptions of Streptococcal associations with colorectal malignancies have been reported in the literature. Streptococcus bovis (Group D streptococci) bacteremia and its association with underlying colon cancer are well known, prompting gastroenterologists to perform colonoscopy if there is evidence of endocarditis. However, the association of GAS with underlying rectal cancer has not been reported in the literature. To our knowledge, this is the first case of GAS bacteremia from a primary GI infection and associated with underlying invasive rectal adenocarcinoma. We postulate that the annexation of the rectal mucosa by adenocarcinoma might have provided the invading organism with access to the bloodstream, leading to bacteremia.
Conclusions: Streptococcus Bovis (Group D streptococci) bacteremia and its association with underlying colorectal cancer is well known. This case underscores the importance of colorectal evaluation in patients with Group A Streptococcal bacteremia presenting with primary gastrointestinal symptoms. An underlying invasive rectal carcinoma could be the inciting cause. Physicians should maintain a high clinical suspicion to hasten diagnosis and allow for prompt treatment.