Background: The transfer of patients between hospitals (interhospital transfer, IHT), exposes patients to risks of discontinuity of care, such as errors in communication and gaps in information transfer. In this study, we aim to quantify clinician-reported medical errors attributable to incomplete communication/information transfer during IHT to a tertiary referral hospital.
Methods: We included all patients transferred from another acute care hospital to the general medicine, cardiology and oncology services at an 800-bed tertiary care facility that accepts over 5000 IHT patients annually. Patients were included if they were transferred between 8/2020-10/2020 (to date). We conducted surveys of admitting clinicians within 48 hours after IHT patient admission, using a daily generated report to identify eligible IHT patients and their corresponding admitting clinicians. Clinicians were emailed instructions to complete a short confidential survey via a REDCap link. Survey questions, based on those from similar studies on patient handoffs, pertained to the clinician’s care of the specific transferred patient and asked about failures in communication (i.e., the presence of inaccurate or missing information) and evaluated for any medical errors (i.e., failures or delays in ordering or interpreting diagnostic studies or delays in therapeutic care). Non-responding clinicians were emailed daily reminders for up to 3 days, with a final personalized email sent by the study’s principal investigator (SM). For this analysis, we descriptively report the frequency and types of clinician-reported failures of communication, and medical errors attributable to incomplete communication/information transfer during IHT, stratified by admitting service.
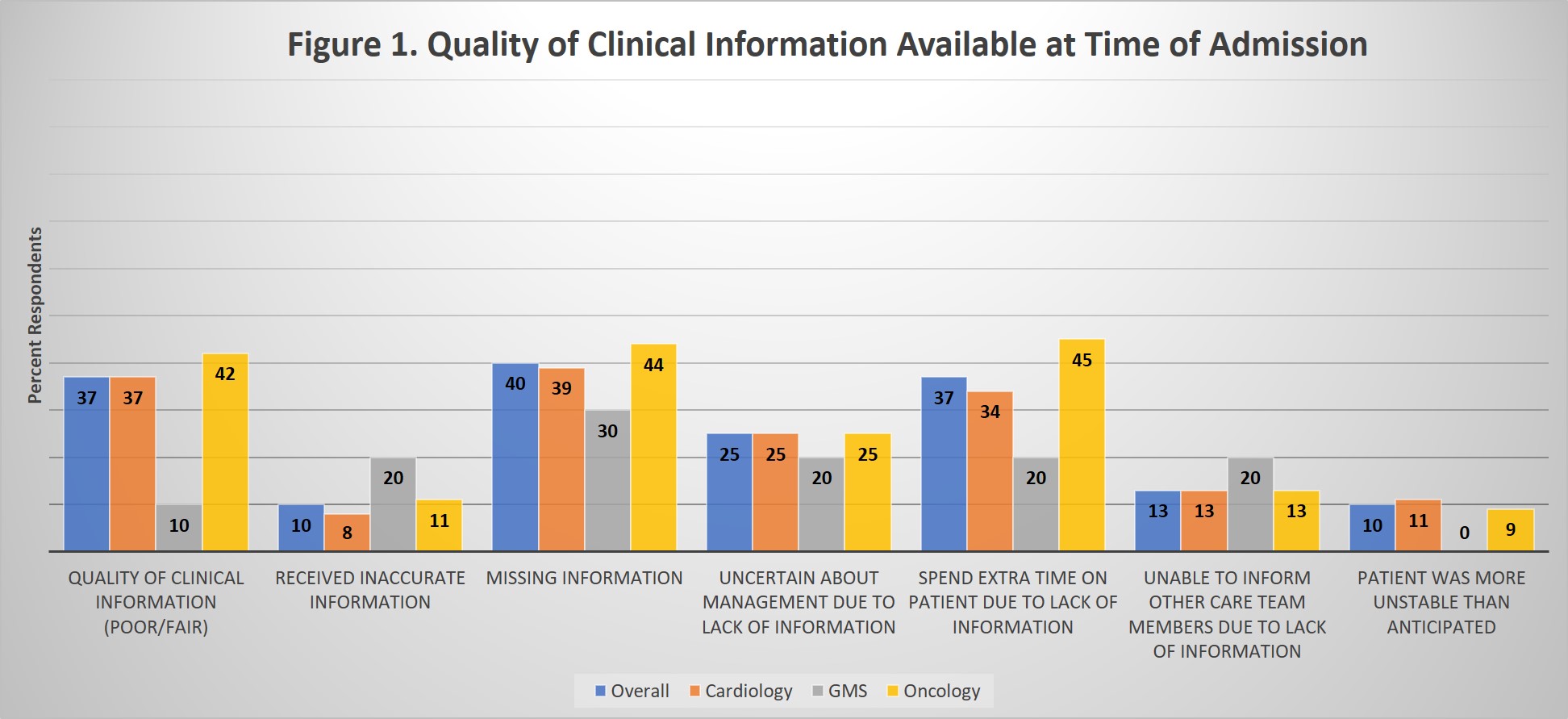
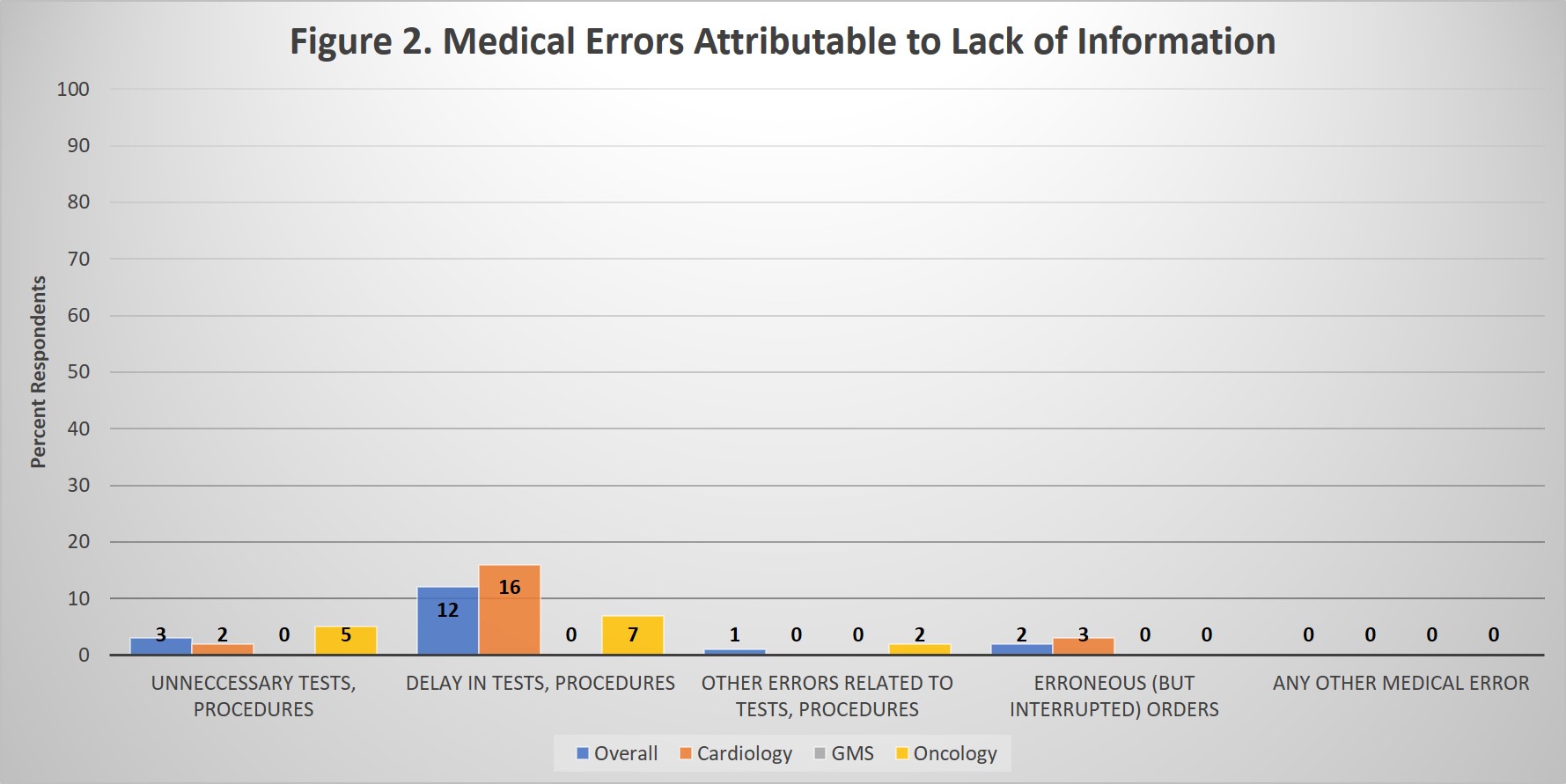
Results: Of the 216 IHT patients transferred to included services to date, admitting clinicians completed surveys on 164 (response rate 76%), including 10 patients transferred to general medicine, 99 to cardiology, and 55 to oncology services. Overall, 37% of respondents reported that the quality of information available at time of IHT was “Poor” or “Fair” and reported needing to spend extra time learning about the patient because they lacked essential clinical information. 40% of respondents reported missing important clinical information, and 25% reported being uncertain about management decisions due to lack of patient information. Results by service are shown (Figure 1). Regarding medical errors, 12% of respondents reported delays in ordering or patient receiving needed tests, procedures, medications, fluids, or other therapies attributable to inaccurate or omitted information available to them at time of admission, primarily among cardiology and oncology IHT patients (Figure 2).
Conclusions: Among a population of IHT patients to a large referral hospital, we found that a substantial number of patients had suboptimal quality of information available at time of IHT. Frontline admitting clinicians frequently reported lacking essential clinical information leading to inefficient workflow, uncertainty about clinical management, and delays in diagnostic or therapeutic care. These findings persisted among all included services but were most notable among higher frequency IHT services (cardiology and oncology). Next steps include utilizing these data and stakeholder input to design, implement and rigorously evaluate a standardized accept note to improve communication during IHT.