Background: Management of heart failure (HF) patients revolves around optimization of guideline directed medical therapy (GDMT) and routine monitoring. Substance use plays a major role as the etiology of HF, especially in a low socioeconomic area with ethnic and racial minority patients. The aim of this study is to find the correlation of alcohol, tobacco and substance use and its impact on their Social Determinants of Health (SDoH) and Burden of Treatment (BoT)
Methods: Patients admitted to Lincoln Medical Center with CHF exacerbation from April 2022 are identified and consented. We used a Patient Experience with Treatment and Self-management (PETS) tool that assessed SDoH and BoT with single item and multiple item domains that includes medical information, medications, medical appointments, health monitoring, relationship, health care expenses, difficulty with health care services, role and social activity limitations, and physical and mental exhaustion for the assessment of BoT and bills and finances, food insecurities, needs for benefits, school, childcare, housing insecurities, housing conditions, immigration, social isolation and homelessness for SDoH. Baseline data also acquired by chart review. The data were analyzed with Mantel-Haenszel.
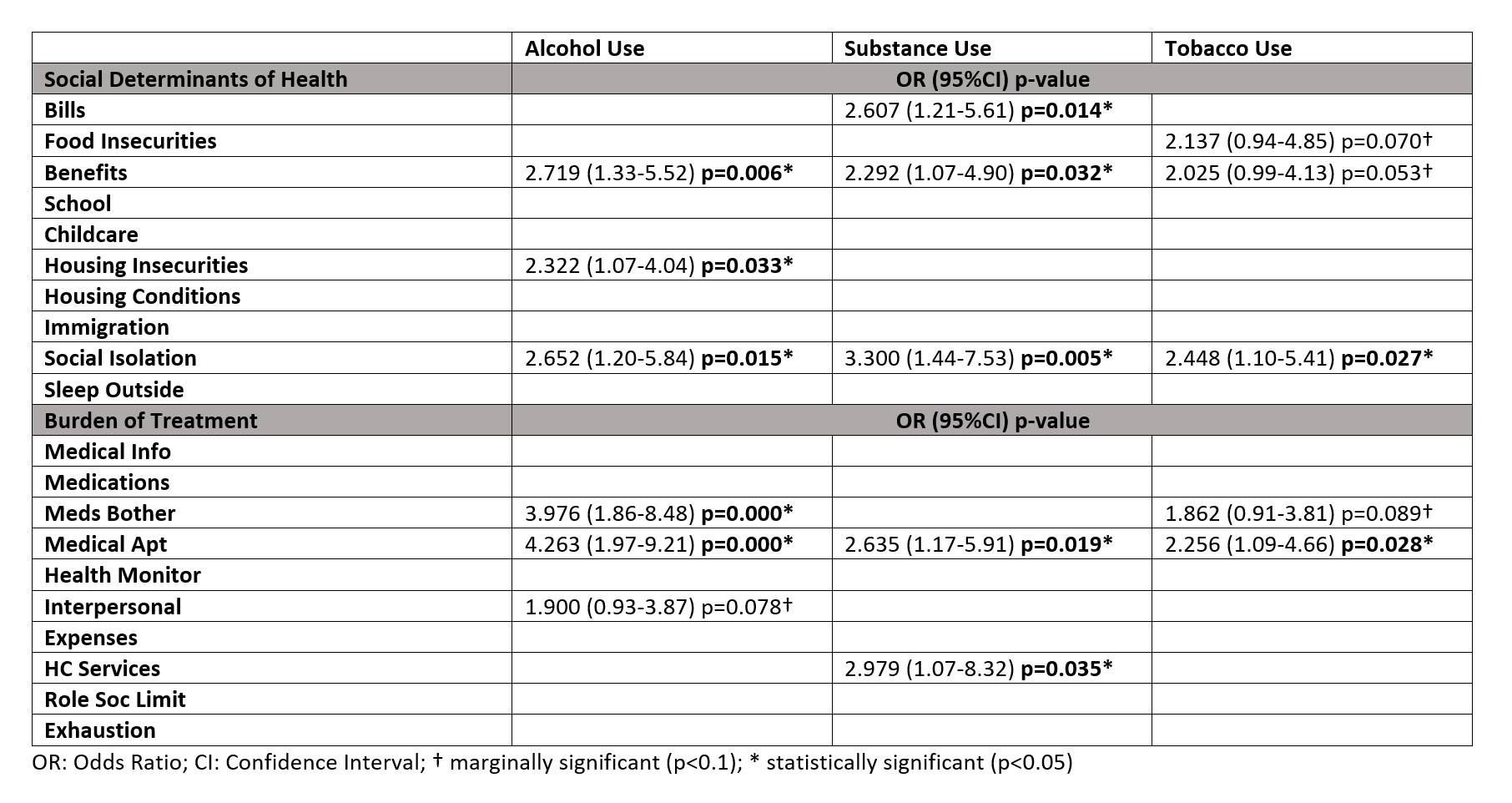
Results: Our patient population has a mean age of 62 years old with 50.3% male. We have 66.4% patients with HF with reduced ejection fraction (HFrEF). Out of all our patients, 30.8% with alcohol use, 23.3% with substance use and 29.6% with tobacco use. In this study, we found that HF patients with alcohol, substance and tobacco use are associated with the SDOH domain of social isolation (respectively, OR=2.652 (95%CI 1.20-5.84) p=0.015; OR=3.300 (95%CI 1.44-7.53) p=0.005; OR=2.448 (95%CI 1.10-5.41) p=0.027). Furthermore, patients with ETOH abuse are associated with the SDOH domains of needing assistance with benefits (OR=2.719 (CI95% 1.33-5.52) p=0.006) and housing insecurities (OR=2.322 (95%CI 1.07-4.04) p=0.033). Patients with substance use are also associated with difficulty paying bills (OR=2.607 (95%CI 1.21-5.61) p=0.014) and needing assistance with benefits (OR=2.292 (95%CI 1.07-4.90) p=0.032). We found marginally significant association with tobacco use with food insecurities (OR=2.137 (95%CI 0.94-4.85) p=0.070) and needing assistance with benefits (OR=2.025 (95%CI 0.99-4.13) p=0.053). For Burden of Treatment, we found that all alcohol, substance and tobacco use are associated with difficulty with keeping and going to medical appointments (Respectively OR=4.263 (95%CI 1.97-9.21) p=0.000; OR=2.635 (95%CI 1.17-5.91) p=0.019; OR=2.256 (95%CI1.09-4.66) p=0.028). Alcohol use patients also has an association with medication bother (OR=3.976 (95%CI 1.86-8.48) p=0.000), while substance use patients are associated with difficulty with healthcare services (OR=2.979 (95%CI 1.07-8.32) p=0.035).
Conclusions: In treating HF patients with alcohol, tobacco and substance use, social isolation should be one of the aspects of SDoH we try to improve as it is directly linked to substance use without HF, such as linkage to group treatment and rehabilitation. Community outreach program could also be deployed to these patients as going to their appointments could lead to decreased rehospitalization and improved prognosis. However, abstinence from substances, although difficult, is still the primary improvement we should aim for.