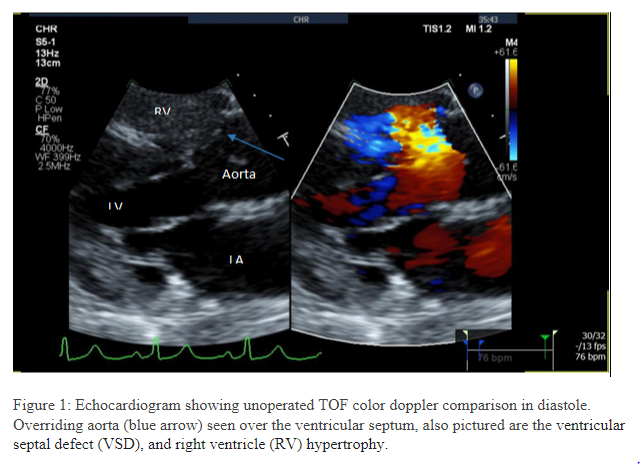
Case Presentation: A 45-year-old female with history of VSD presented with fever and fatigue. She had a systolic ejection murmur with palpable thrill best heard at the second intercostal space. Echocardiographic findings included severe RV hypertrophy (1.7 cm thick), infundibular pulmonary obstruction, perimembranous VSD (1.4×0.6 cm), and mobile tricuspid valve echodensities (Figure 1). Blood cultures confirmed Strep. parasanguinis endocarditis.Cardiothoracic surgeons deemed corrective TOF surgery imperative, but a lack of insurance made it unaffordable. She received treatment for endocarditis and was discharged for outpatient care which has been sparse due to her uninsured status.
Discussion: Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease, affecting about one in 2,518 U.S. newborns yearly. It includes four key defects: overriding aorta, right ventricular outflow obstruction (RVOT), VSD, and right ventricular (RV) hypertrophy. Early surgery is critical, due to high mortality in unoperated cases: 1-year survival at 66%, 3-year at 49%, and less than 2% past the age of 40.
Conclusions: The patient’s exceptional longevity is due to well-balanced hemodynamics. Her infundibular stenosis primarily directs right ventricular volume into the pulmonary circulation and left ventricular volume into the ascending aorta, even with a large VSD. This stability is evidenced by her absence of cyanosis, a hemoglobin level of 14 g/dl, and arterial oxygen saturation of 96%, allowing her to survive against the odds.